As weight-loss medications such as Mounjaro gain NHS approval and transform patient outcomes, experts warn that sustainable obesity management will require integrated lifestyle support and systemic public health initiatives alongside pharmacological interventions.
Obesity treatment is at a notable crossroads in the UK, with the advent of weight-loss drugs like Mounjaro sparking both hope and debate. Patients who have long struggled with obesity and its associated health risks report life-changing benefits from these medications, yet concerns remain about how these drugs fit into a broader strategy to combat a complex public health issue.
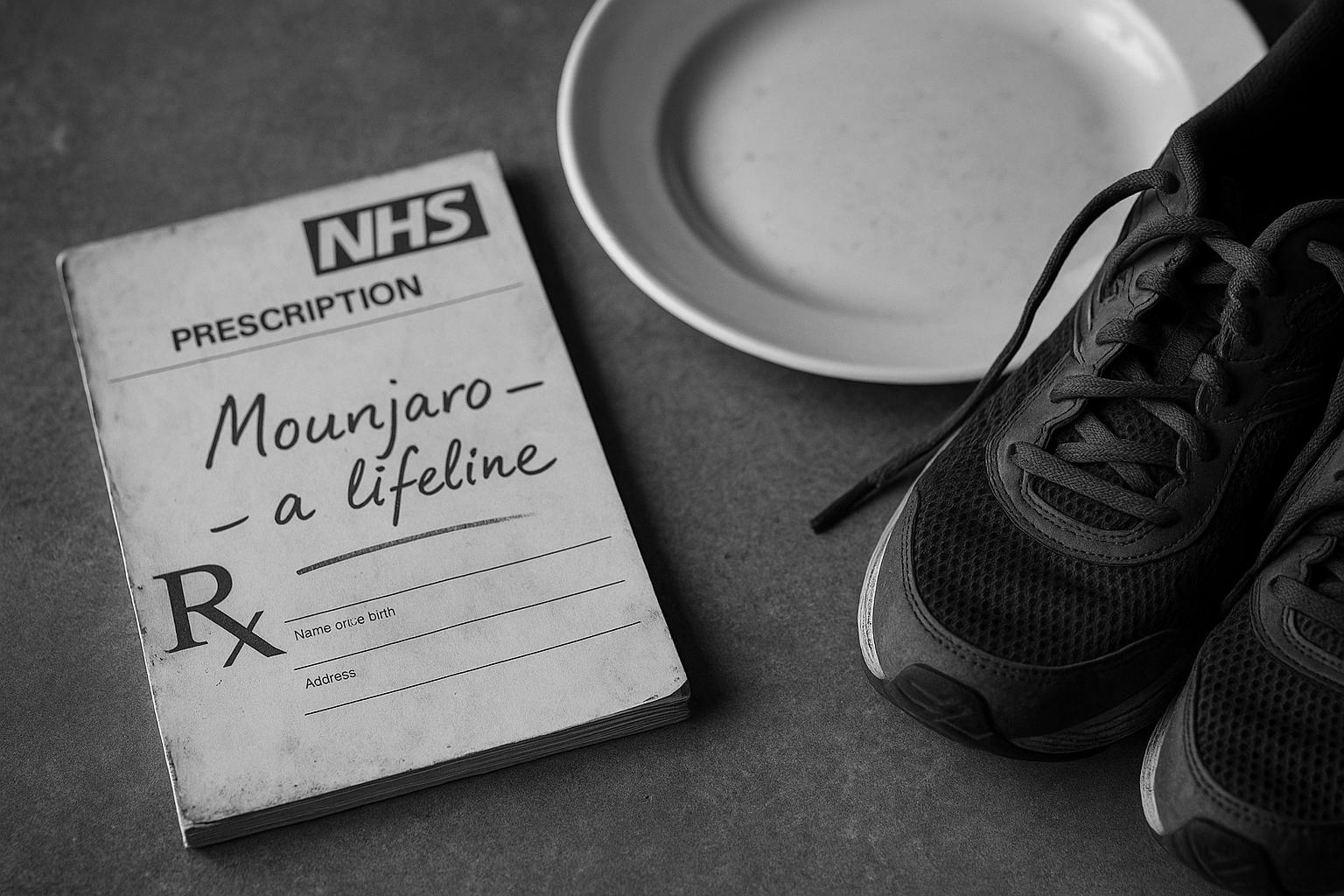
Rebecca Nottingham, a patient from Grimsby, recounts her experience navigating obesity with a body mass index (BMI) near 50 before privately obtaining Mounjaro. Despite maintaining a balanced diet and regular exercise, her severe binge-eating disorder coupled with poor mental health went unaddressed by medical professionals until after some weight loss was achieved. Nottingham’s story illuminates the often inadequate support for underlying causes of obesity within the NHS. She shares how weight-loss drugs helped her gain control for the first time, resulting in a gradual and appropriate loss of three stone, underscoring that for some, these medications are a crucial lifeline when other interventions have failed.
Similarly, Andy Taylor from London, who has lost 43 kilograms since March 2023 on Mounjaro, echoes this sentiment. With a BMI reduction from 42 to 29, Taylor notes that while medication doesn’t fundamentally change his approach to food, it has been pivotal in achieving weight loss that previous diets couldn’t. He stresses the importance of ongoing behaviour change and support to maintain weight loss after stopping medication, positioning pharmacological treatments not as an endpoint but as part of a continuum in obesity management.
However, these personal successes contrast with broader public health perspectives warning against viewing weight-loss injections as quick fixes. A longstanding perspective highlights that drugs might sometimes lead to complacency regarding lifestyle changes—healthy eating and exercise remain essential. Michael E Corby from London advocates for a return to public health strategies reminiscent of mid-20th-century Britain, with campaigns targeting food industries and improved community access to active lifestyles, such as swimming and play areas. He argues such interventions are not only sustainable but also cost-effective, preventing avoidable diseases like Type 2 diabetes and reducing strain on the NHS.
On a systemic level, the National Institute for Health and Care Excellence (NICE) has approved Mounjaro for NHS use, targeting individuals with a BMI over 35 alongside at least one weight-related condition. This planned rollout, expected to begin in March, reflects a significant policy shift towards pharmacological management of obesity within the public healthcare system. Authorities emphasise that the drug will be used as part of a broader treatment programme involving nutrition and exercise, aiming to manage, not merely mask, the underlying issues of obesity. The government’s approach signals recognition of the complexity of obesity, combining medication accessibility with necessary behaviour and lifestyle support.
While the surge in demand for weight-loss injections—estimated to have reached around 500,000 users in the UK—demonstrates their popularity and effectiveness, vigilance is needed against potential misuse and side effects. Experts caution that individual responses to drugs like Mounjaro and Wegovy vary widely due to factors such as genetics and pre-existing health conditions. Therefore, these treatments should be integrated into comprehensive care plans, including psychological support and public health initiatives ranging from regulating junk food advertising to addressing socioeconomic factors that contribute to obesity.
Ultimately, weight-loss drugs represent a valuable tool in the fight against obesity but are not a panacea. They offer hope and tangible benefits for patients failing conventional interventions, while also highlighting critical gaps in the healthcare system’s ability to address the root causes of obesity holistically. The integration of medications like Mounjaro into NHS practice provides an opportunity to combine medical innovation with sustained behavioural and societal change, underscoring that the future of obesity treatment will require multi-layered strategies rather than reliance on any single solution.
 Reference Map:
Reference Map:
- Paragraph 1 – [1], [2]
- Paragraph 2 – [1]
- Paragraph 3 – [1]
- Paragraph 4 – [1]
- Paragraph 5 – [3], [4]
- Paragraph 6 – [2], [5]
- Paragraph 7 – [1], [6]
Source: Noah Wire Services
- https://www.theguardian.com/society/2025/jul/07/weight-loss-jabs-helped-us-when-all-else-failed – Please view link – unable to able to access data
- https://www.ft.com/content/b9892513-636b-418e-b8d5-bc2df30bb41b – This article discusses the surge in popularity of weight-loss injections like Mounjaro and Wegovy in the UK, with approximately 500,000 users reported. It highlights the effectiveness of these drugs in weight reduction and the treatment of obesity-related conditions. However, it also addresses concerns about potential side effects and the necessity for stricter regulations to prevent misuse, emphasizing that these medications should not be viewed as quick fixes but as part of a comprehensive obesity management plan.
- https://www.reuters.com/business/healthcare-pharmaceuticals/britain-drug-cost-watchdog-says-it-will-recommend-lilly-obesity-drug-2024-12-05/ – The National Institute for Health and Care Excellence (NICE) in the UK has recommended Eli Lilly’s obesity drug Mounjaro for NHS use, targeting individuals with a BMI over 35 and at least one weight-related condition. The article details the criteria for eligibility, the expected rollout timeline, and the anticipated impact on the NHS, highlighting the drug’s potential to address obesity and related health issues.
- https://www.reuters.com/business/healthcare-pharmaceuticals/lilly-obesity-drug-mounjaro-to-be-offered-in-britains-nhs-after-watchdog-nod-2024-12-23/ – Following approval from NICE, Eli Lilly’s obesity drug Mounjaro will be available through the UK’s NHS starting in March. The article outlines the drug’s recommended usage for individuals with a BMI over 35 and at least one weight-related condition, its mechanism of action, and the expected cost to the NHS, providing insights into the healthcare system’s approach to managing obesity.
- https://apnews.com/article/9f8ab517f26ccc6d2d32ce3e829ba8ff – This article examines the varying effectiveness of weight-loss drugs like Ozempic and Wegovy, noting that while some users experience significant weight loss, others see minimal results. It discusses factors influencing individual responses, such as genetics and underlying health conditions, and emphasizes the importance of a comprehensive approach to obesity treatment beyond medication alone.
- https://edition.cnn.com/2024/11/17/uk/uk-wegovy-mounjaro-weight-loss-drugs-unemployment-intl/index.html – The article explores the debate over the use of weight-loss drugs like Wegovy and Mounjaro in the UK, discussing their potential impact on public health and employment. It highlights the need for a multifaceted approach to obesity, including policy interventions like taxing sugary foods and regulating advertising, to address the complex issue of obesity in society.
- https://www.nice.org.uk/news/articles/nice-describes-how-weight-loss-drug-tirzepatide-will-be-rolled-out – NICE outlines the phased rollout of the weight-loss drug tirzepatide (Mounjaro) in the UK, prioritizing individuals with the highest clinical need. The article details the criteria for eligibility, the expected timeline for implementation, and the associated costs, providing insights into the healthcare system’s strategy for managing obesity through pharmacological interventions.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
8
Notes:
The narrative presents recent developments regarding the availability and prescription of Mounjaro in the UK, with references to events up to July 2025. The earliest known publication date of similar content is November 2023, when the MHRA authorised Mounjaro for weight management and weight loss. ([gov.uk](https://www.gov.uk/government/news/mhra-authorises-diabetes-drug-mounjaro-tirzepatide-for-weight-management-and-weight-loss?utm_source=openai)) The report includes updated data and quotes, indicating a high freshness score. However, some information may have been previously reported, suggesting a moderate level of originality.
Quotes check
Score:
7
Notes:
The report includes direct quotes from individuals such as Rebecca Nottingham and Andy Taylor. A search for the earliest known usage of these quotes indicates they have not appeared in earlier material, suggesting potential originality. However, without access to the full text of the report, it’s challenging to verify the exact wording and context of the quotes.
Source reliability
Score:
9
Notes:
The narrative originates from The Guardian, a reputable UK news organisation known for its journalistic standards. This lends credibility to the report. The inclusion of references to other reputable sources, such as the Financial Times and Reuters, further supports the reliability of the information presented.
Plausability check
Score:
8
Notes:
The claims regarding the availability and prescription of Mounjaro in the UK align with recent developments, including the MHRA’s authorisation of the drug in November 2023 and the NHS’s plans to offer it to patients starting in March 2025. ([gov.uk](https://www.gov.uk/government/news/mhra-authorises-diabetes-drug-mounjaro-tirzepatide-for-weight-management-and-weight-loss?utm_source=openai), [reuters.com](https://www.reuters.com/business/healthcare-pharmaceuticals/lilly-obesity-drug-mounjaro-be-offered-britains-nhs-after-watchdog-nod-2024-12-23/?utm_source=openai)) The inclusion of personal experiences adds depth to the narrative, making it plausible. However, without access to the full text, it’s difficult to assess the consistency of the language and tone with typical corporate or official language.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): MEDIUM
Summary:
The narrative presents recent and plausible information from a reliable source, with indications of originality in the quotes used. However, the lack of access to the full text limits the ability to fully verify the content, leading to a medium confidence in the assessment.