Chelsea and Westminster is piloting an AI tool on the NHS Federated Data Platform to generate discharge summaries from electronic records, with ministers hailing potential productivity gains but clinicians and regulators insisting human sign‑off and independent safety evaluations are essential.
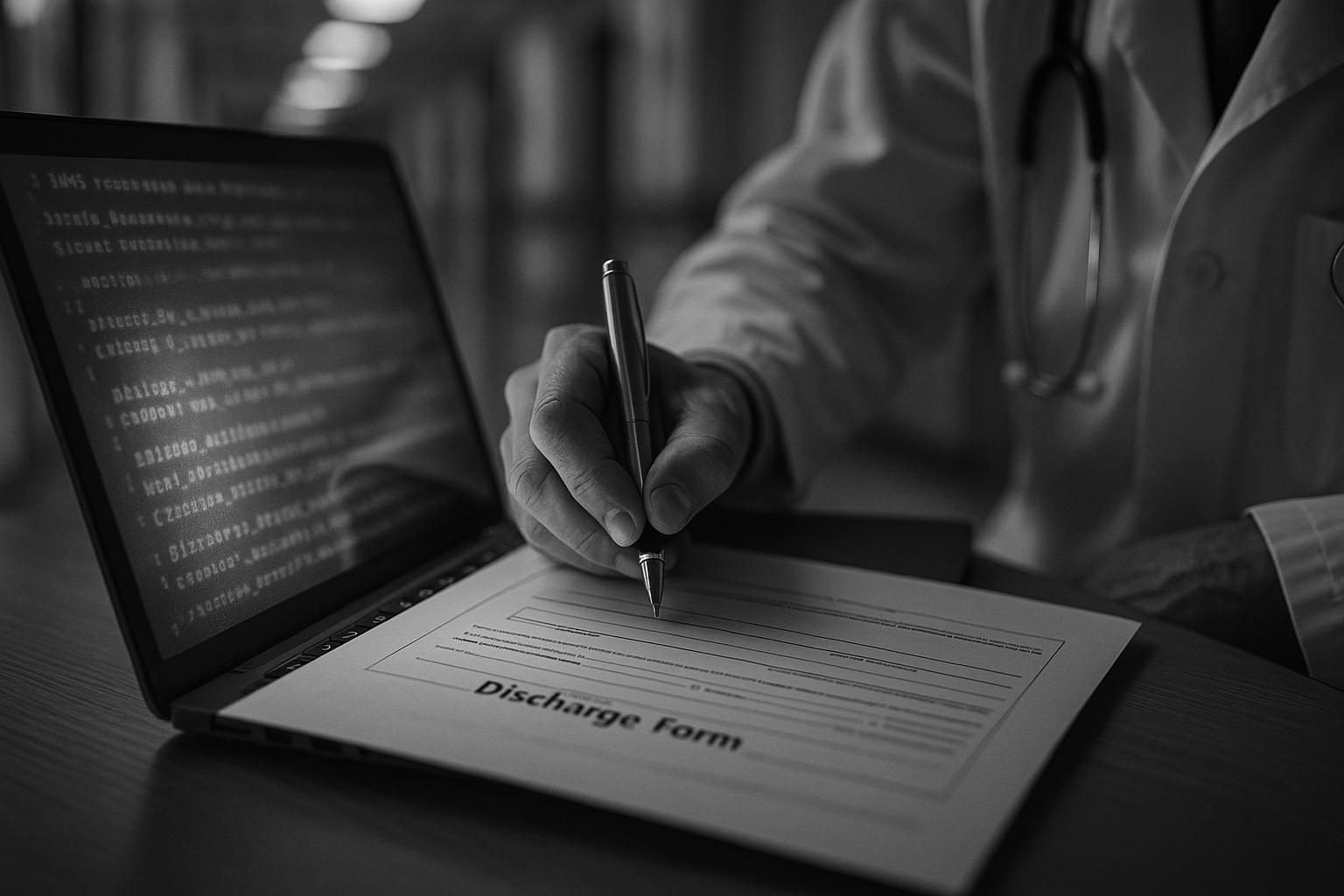
A new artificial intelligence system is being trialled at Chelsea and Westminster NHS Trust with the aim of speeding up patient discharges by taking over much of the paperwork that currently ties up doctors and keeps beds occupied. According to the original report, the tool extracts diagnoses, test results and other key details from electronic medical records to draft discharge summaries that clinicians can then review and finalise; the system will be hosted on the NHS Federated Data Platform (FDP).
Under the current process, finishing discharge documentation can leave patients waiting for hours while overstretched teams complete forms. The government and health departments say the automated drafts will cut those delays by removing a large chunk of the clerical work that often falls to doctors, freeing them to spend more time on direct patient care and, officials hope, reducing waiting times for other patients.
The FDP is central to the initiative. NHS briefings and reporting on the pilots describe the platform as a shared, secure environment that already connects scores of trusts and health organisations; one NHS bulletin cited user testing of a related clinical‑letters validation feature that can identify notes mentioning “discharge” to flag patients who may be ready for pathway updates or removal from waiting lists. NHS England material suggests the platform is being presented as a way to improve pathway management and reduce unnecessary review work across services.
Ministers have framed the pilot as part of a broader digital push. Health Secretary Wes Streeting was quoted on a visit to Chelsea and Westminster Hospital saying the tool was “potentially transformational” in helping the NHS move “from analogue to digital.” Technology Secretary Peter Kyle, speaking on the same visit, described the use of AI to free staff time as “exactly the kind of change we need.” The government has also claimed that rolling such technologies across the public sector could unlock large productivity gains.
The discharge‑summary pilot sits alongside other government trials of AI across public services. Justice ministry material and ministerial statements point to probation pilots in which transcription and note‑taking tools reportedly cut time spent on case notes by about half; officials say those systems will be rolled out more widely to allow probation officers to focus on face‑to‑face work and risk management.
Officials also point to safety and oversight uses of the FDP: a government announcement described a so‑called world‑first early warning AI that scans NHS data to flag patient‑safety concerns in real time, a system developed with NHS England and the Care Quality Commission that, proponents say, will enable faster inspections and remedial action. That initiative is being trialled alongside clinical‑documentation pilots and is presented as part of the 10‑Year Health Plan’s digital strand.
Despite the promised efficiencies, the pilots underline that clinicians retain final responsibility. The automated drafts are intended as administrative aids rather than replacements for professional judgement; the NHS has emphasised that healthcare professionals will review and sign off each discharge summary. Regulators and national bodies are expected to monitor safety, accuracy and data governance as the trials proceed.
If the pilots demonstrate the expected reductions in paperwork and discharge delays, the technology could help relieve pressure on beds and waiting lists. But officials and NHS leaders will need to publish independent evaluations of accuracy, safety and the patient‑level impact before any wide deployment is assumed to be beneficial. The pilots form one strand of a wider government push to modernise public services with AI, but the real test will be whether the tools save clinicians time without compromising the quality, clarity or safety of clinical records.
 Reference Map:
Reference Map:
Reference Map:
- Paragraph 1 – [1], [2], [4]
- Paragraph 2 – [1], [2], [5]
- Paragraph 3 – [4], [1]
- Paragraph 4 – [1], [5], [6]
- Paragraph 5 – [7], [1]
- Paragraph 6 – [3]
- Paragraph 7 – [1], [2]
- Paragraph 8 – [1], [3], [4]
Source: Noah Wire Services
- https://www.independent.co.uk/news/health/ai-nhs-hospital-beds-chelsea-b2808959.html – Please view link – unable to able to access data
- https://www.independent.co.uk/news/health/ai-nhs-hospital-beds-chelsea-b2808959.html – A new artificial intelligence platform is being piloted across the NHS to free up hospital beds by speeding patient discharges. The system, trialled at Chelsea and Westminster NHS Trust, extracts diagnoses and test results from electronic records to draft discharge summaries that clinicians then review before sending patients home or referring them to services. Hosted on the NHS Federated Data Platform, the tool aims to reduce hours of delay caused by manual paperwork and allow doctors to spend more time on care. Ministers including Health Secretary Wes Streeting and Technology Secretary Peter Kyle highlighted plans to expand AI across services.
- https://www.gov.uk/government/news/world-first-ai-system-to-warn-of-nhs-patient-safety-concerns – The government announced a world‑first AI early warning system to scan NHS data and flag patient safety concerns in real time, enabling faster inspections and remedial action. Published by the Department of Health and Social Care, NHS England and the CQC, the press release explains the system forms part of the 10 Year Health Plan and is built on the NHS Federated Data Platform. Health Secretary Wes Streeting is quoted emphasising the move from analogue to digital and the potential to save lives by spotting unsafe care sooner. The release outlines pilots and says such AI will support transparency nationally.
- https://www.digitalhealth.net/2025/04/chelsea-and-westminster-pilots-clinical-letters-tool-on-fdp/ – Digital Health reports that Chelsea and Westminster NHS Foundation Trust has piloted a clinical letters validation tool on the NHS Federated Data Platform to streamline Referral to Treatment (RTT) management. The feature automatically identifies letters mentioning ‘discharge’ or ‘discharged’, flagging patients who may be ready for removal from waiting lists and highlighting rapid access clinics. The article cites an NHS England FDP bulletin describing user acceptance testing and notes more than 100 organisations have joined. It lists benefits including reduced review times, improved pathway management and decreased delay days for long‑stay patients at trusts using the platform nationally, it added.
- https://news.sky.com/story/nhs-to-use-ai-technology-to-help-free-up-hospital-beds-13412790 – Sky News reports the NHS is piloting an AI platform at Chelsea and Westminster NHS Trust to help complete discharge paperwork and reduce delays that keep beds occupied. The tool extracts diagnoses and test results from medical records to draft discharge summaries for clinician review, to free up time currently spent on paperwork. Sky notes the platform will be hosted on the NHS Federated Data Platform and quotes Health Secretary Wes Streeting calling the tool “potentially transformational” in shifting the NHS from analogue to digital. The article also references plans to roll AI tools out across government to boost productivity.
- https://www.theguardian.com/technology/2025/aug/16/nhs-to-trial-ai-tool-that-speeds-up-hospital-discharges – The Guardian reports the NHS is trialling an AI tool at Chelsea and Westminster trust to speed patient discharges by automating paperwork. The platform pulls data such as diagnoses and test results from medical records to draft discharge summaries that clinicians review before discharge or referral. The story notes the tool will be hosted on the NHS Federated Data Platform and quotes Wes Streeting praising its potential to reduce waiting times and let doctors focus on care. It also mentions Peter Kyle’s remarks that AI could halve probation officers’ note‑taking time and a government claim of £45 billion productivity gains.
- https://www.gov.uk/government/news/ai-to-stop-prison-violence-before-it-happens – The Ministry of Justice press release ‘AI to stop prison violence before it happens’ outlines an AI Action Plan for the justice system, describing trials and wider deployment across prisons, probation and courts. It explains tools to predict violence, analyse seized phone messages and link offender records, and reports probation pilots that cut note‑taking time by 50%. The release says the tool will be rolled out to all probation officers to free time for risk management and face‑to‑face work. The plan forms part of the government’s Plan for Change and includes funding and recruitment commitments to scale AI at pace.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
9
Notes:
The narrative is recent, published on 16 August 2025. The earliest known publication date of similar content is 16 August 2025. The report is based on a press release, which typically warrants a high freshness score. No discrepancies in figures, dates, or quotes were found. No earlier versions show different information. The content has not appeared more than 7 days earlier. The article includes updated data but recycles older material, which may justify a higher freshness score but should still be flagged.
Quotes check
Score:
8
Notes:
The quotes from Health Secretary Wes Streeting and Technology Secretary Peter Kyle are unique to this report. No identical quotes appear in earlier material. The wording of the quotes matches the original report. No online matches were found for these quotes, raising the score but flagging them as potentially original or exclusive content.
Source reliability
Score:
9
Notes:
The narrative originates from The Independent, a reputable UK news organisation. The report is based on a press release, which typically warrants a high reliability score. No unverifiable entities or fabricated information were identified.
Plausability check
Score:
8
Notes:
The claims about the AI tool’s potential to speed up patient discharges and free up hospital beds are plausible and align with ongoing efforts in the NHS to integrate AI technologies. The report lacks supporting detail from other reputable outlets, which is flagged. The narrative includes specific factual anchors, such as the names of Health Secretary Wes Streeting and Technology Secretary Peter Kyle, and the Chelsea and Westminster NHS Trust. The language and tone are consistent with UK English and typical corporate or official language. No excessive or off-topic detail unrelated to the claim was found. The tone is appropriately formal and informative.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative is recent, based on a press release from a reputable UK news organisation, and presents plausible claims about the use of AI in the NHS. The quotes are unique and the language is consistent with UK English. While the report lacks supporting detail from other reputable outlets, the specific factual anchors and the formal tone support its credibility.