Recent research uncovers that antibiotic resistance predates modern medicine by millions of years, with ancient bacteria exhibiting mechanisms similar to today’s drug-resistant pathogens. Understanding this evolutionary history offers vital insights for combating the ongoing global health crisis caused by antibiotic resistance.
Understanding the Evolution of Antibiotic Resistance: Lessons from the Past
Antibiotics are celebrated as one of the hallmark achievements of modern medicine, fundamentally transforming the management of infectious diseases since their inception in the 1940s. These powerful agents have not only improved health outcomes but also significantly extended life expectancy. However, the emergence of antibiotic resistance poses a dire threat to this medical revolution, complicating treatment options and prompting a global health crisis.
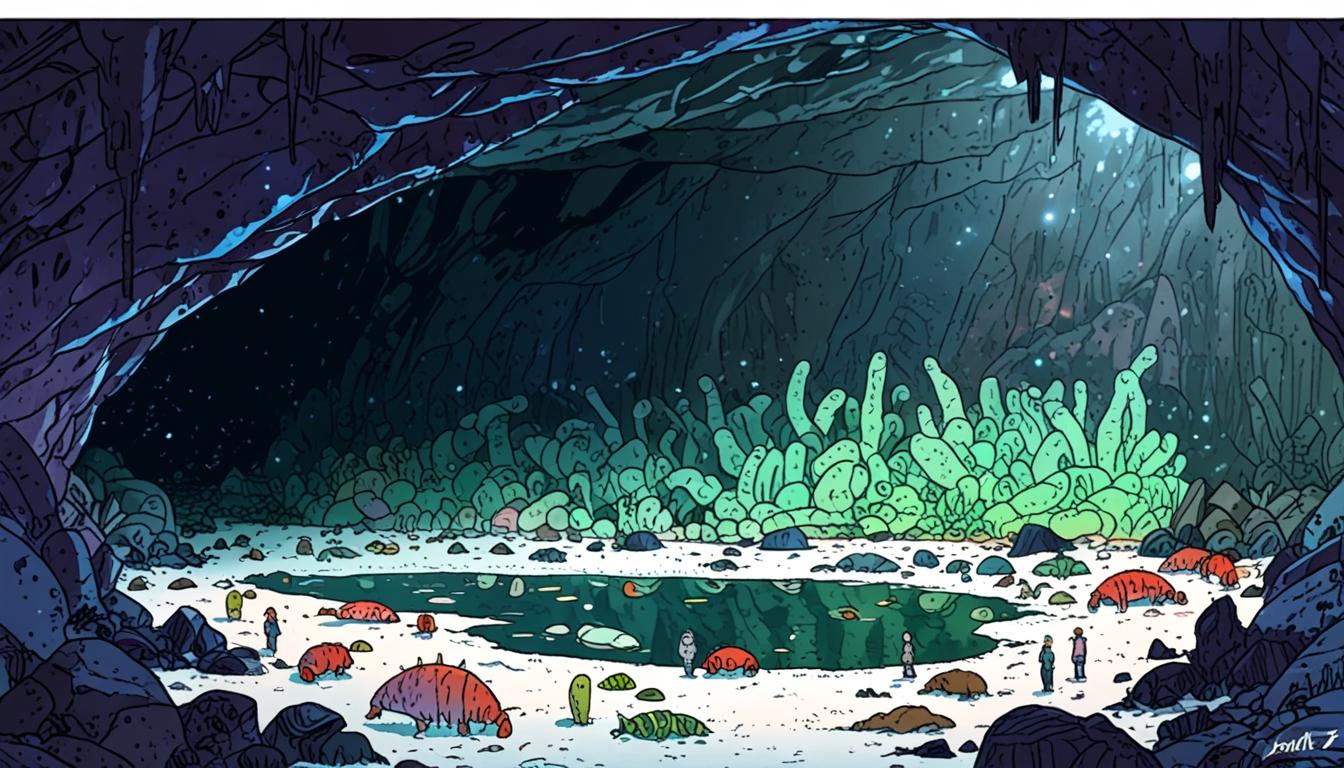
Recent insights reveal that antibiotic resistance is not merely a contemporary challenge; it is an intricate and deeply-rooted evolutionary phenomenon that predates the clinical use of antibiotics. Bacteria evolved resistance mechanisms long before these drugs were discovered, indicating a complex lineage that intertwines with the natural history of microbial organisms. For example, studies have identified antibiotic-resistant bacteria in untouched environments, such as ancient permafrost and isolated caves, suggesting that resistance traits have been conserved over millennia.
Research indicates that the genetic material responsible for antibiotic resistance has been found in samples dating back as far as 30,000 years, with some strains exhibiting resistance profiles remarkably similar to modern pathogens. Staphylococcus strains isolated from 3.5 million-year-old permafrost samples have shown resilience against a range of antibiotics, including β-lactams and vancomycin. Such findings highlight the astonishing longevity of these resistance genes and their adaptive significance in harsh ecological settings.
Interestingly, analysis of the Lechuguilla Cave in New Mexico, which has remained unaltered by human activity for approximately four million years, uncovered the presence of Streptomyces and Paenibacillus species with striking similarities to current antibiotic-resistant strains. This suggests that resistance mechanisms are not only ancient but also integral to the survival strategies of bacteria throughout history. In fact, a 2022 study revealed that certain strains of methicillin-resistant Staphylococcus aureus were already adaptable to antibiotic challenges long before the introduction of methicillin, having evolved in response to environmental pressures, including interactions with antibiotic-producing fungi prevalent in their ecological niches.
The evolutionary dynamics of antibiotic resistance can be understood in the context of fierce competition and adaptation. In the absence of modern antibiotics, natural compounds played crucial roles in microbial communities by inhibiting competitor growth, thus fostering the proliferation of antibiotic-producing species. This ecological competition laid the groundwork for bacterial defence mechanisms to thrive, escalating the diversification of resistance strategies over eons. The mechanisms utilized by modern pathogens mirror those found in these ancient ecosystems, underscoring the importance of studying historical resistance to inform our strategies against contemporary antibiotic challenges.
The transfer of resistance genes appears to occur randomly, often from environmental microbes to human commensals, and subsequently to pathogenic bacteria. The prevalence of a particular resistance mechanism in the environment increases the likelihood of its transfer, which implies that reservoirs of resistance can accelerate the evolution of multiple drug-resistant pathogens under antibiotic pressure. Understanding this gene flow is vital for developing effective interventions and upholding public health.
Reflecting on the past is crucial for predicting future trajectories of antibiotic resistance. By uncovering the evolutionary history of resistance genes, scientists can better anticipate how they might evolve in response to ongoing antibiotic use. This knowledge equips researchers and healthcare professionals with the tools to forecast potential resistance mechanisms and adapt strategies accordingly.
As Winston Churchill aptly noted, “the longer you can look back, the further you can look forward.” This perspective emphasises the necessity of examining historical resistance to navigate the complexities of current antibiotic resistance crises. In doing so, we can harness insights from ancient microbial history to devise innovative approaches for combating the relentless rise of drug-resistant infections, ultimately safeguarding public health for future generations.
Reference Map:
- Paragraph 1 – [[1]](https://news.google.com/rss/articles/CBMixwFBVV95cUxORHNCM0ZEaE1LNEU5MmN3UDlhc1A2Zmdsc0g4bFVxWnhGZFE0Qlo2cm9haVAxVHBpLUNoSUdtUG9zb1FzYksyMno4blZheVluY2hOeVR0aXFpemRxcktmSFBzY0QweXZ4WHNGa24tUnNjWFdUaTZPMkQ2TGFUTW9laXBpZnVSZnlROGFuTlh4VnVFM201VUFfeV9ieTJTY1ljdmRxYzJnVkpnZl9mQW9ZSkU5Q0VpblhIT1NPUE1QSjRZQXc3ZzNV?oc=5&hl=en-US&gl=US&ceid=US:en), [[2]](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5052414/)
- Paragraph 2 – [[1]](https://news.google.com/rss/articles/CBMixwFBVV95cUxORHNCM0ZEaE1LNEU5MmN3UDlhc1A2Zmdsc0g4bFVxWnhGZFE0Qlo2cm9haVAxVHBpLUNoSUdtUG9zb1FzYksyMno4blZheVluY2hOeVR0aXFpemRxcktmSFBzY0QweXZ4WHNGa24tUnNjWFdUaTZPMkQ2TGFUTW9laXBpZnVSZnlROGFuTlh4VnVFM201VUFfeV9ieTJTY1ljdmRxYzJnVkpnZl9mQW9ZSkU5Q0VpblhIT1NPUE1QSjRZQXc3ZzNV?oc=5&hl=en-US&gl=US&ceid=US:en), [[3]](https://www.nature.com/articles/s41598-019-57020-6), [[4]](https://www.sciencedirect.com/science/article/pii/S0092867420306785)
- Paragraph 3 – [[4]](https://www.sciencedirect.com/science/article/pii/S0092867420306785), [[5]](https://www.frontiersin.org/articles/10.3389/fmicb.2017.01137/full)
- Paragraph 4 – [[3]](https://www.nature.com/articles/s41598-019-57020-6), [[6]](https://www.cell.com/current-biology/fulltext/S0960-9822(19)31948-1)
- Paragraph 5 – [[6]](https://www.cell.com/current-biology/fulltext/S0960-9822(19)31948-1), [[7]](https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance)
- Paragraph 6 – [[1]](https://news.google.com/rss/articles/CBMixwFBVV95cUxORHNCM0ZEaE1LNEU5MmN3UDlhc1A2Zmdsc0g4bFVxWnhGZFE0Qlo2cm9haVAxVHBpLUNoSUdtUG9zb1FzYksyMno4blZheVluY2hOeVR0aXFpemRxcktmSFBzY0QweXZ4WHNGa24tUnNjWFdUaTZPMkQ2TGFUTW9laXBpZnVSZnlROGFuTlh4VnVFM201VUFfeV9ieTJTY1ljdmRxYzJnVkpnZl9mQW9ZSkU5Q0VpblhIT1NPUE1QSjRZQXc3ZzNV?oc=5&hl=en-US&gl=US&ceid=US:en), [[2]](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5052414/)
Source: Noah Wire Services
- https://news.google.com/rss/articles/CBMixwFBVV95cUxORHNCM0ZEaE1LNEU5MmN3UDlhc1A2Zmdsc0g4bFVxWnhGZFE0Qlo2cm9haVAxVHBpLUNoSUdtUG9zb1FzYksyMno4blZheVluY2hOeVR0aXFpemRxcktmSFBzY0QweXZ4WHNGa24tUnNjWFdUaTZPMkQ2TGFUTW9laXBpZnVSZnlROGFuTlh4VnVFM201VUFfeV9ieTJTY1ljdmRxYzJnVkpnZl9mQW9ZSkU5Q0VpblhIT1NPUE1QSjRZQXc3ZzNV?oc=5&hl=en-US&gl=US&ceid=US:en – Please view link – unable to able to access data
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5052414/ – This article discusses the history and evolution of antibiotic resistance, highlighting the significance of antibiotics, which marked a turning point in modern medicine. It outlines how bacteria have always possessed resistance mechanisms, predating the clinical use of antibiotics. This suggests that antibiotic resistance is a natural phenomenon rooted in evolutionary processes. The study further emphasizes the environmental reservoirs of resistant bacteria and their implications for public health. Research on ancient resistance genes provides insight into resistance mechanisms, showing the importance of understanding the past to address current antibiotic challenges.
- https://www.nature.com/articles/s41598-019-57020-6 – This research highlights the discovery of antibiotic-resistant bacteria in ancient environments, including permafrost and isolated caves. The study found that resistance genes from 30,000-year-old samples are similar to contemporary antibiotic-resistant strains. It discusses how these findings offer insight into bacterial adaptation and the evolutionary basis for resistance, pointing out the significance of ancient bacterial communities in understanding current issues with antibiotic resistance. The data suggests that studying these ancient resistance mechanisms can inform strategies to combat modern bacterial threats effectively.
- https://www.sciencedirect.com/science/article/pii/S0092867420306785 – This article evaluates the evolutionary dynamics of antibiotic resistance, asserting that resistance genes have evolved long before the advent of modern antibiotics. It emphasizes that bacterial competition and natural antibiotics significantly influenced resistance mechanisms. The findings indicate that ancient environments served as reservoirs for resistance genes, facilitating their transmission to human pathogens. Understanding this evolutionary aspect is crucial to developing effective interventions against antibiotic-resistant infections. The connection between ancient resistance and current challenges provides a framework for addressing the public health crisis in antibiotic resistance.
- https://www.frontiersin.org/articles/10.3389/fmicb.2017.01137/full – This Frontiers article focuses on the role of environmental bacteria in antibiotic resistance, showcasing how these microorganisms have adapted to survival challenges through evolutionary history. It details the mechanisms of resistance found in pre-antibiotic environments and emphasizes the importance of these findings in understanding the contemporary rise of resistance in pathogenic bacteria. It argues that insights from ancient microbial resistance can guide future research and strategies in combating antibiotic resistance, reaffirming the necessity of investigating microbial evolution in shaping public health strategies.
- https://www.cell.com/current-biology/fulltext/S0960-9822(19)31948-1 – This Current Biology review explores the ecological and evolutionary contexts of antibiotic resistance, connecting past resistance mechanisms to current public health crises. It discusses how ancient resistance genes, preserved in diverse environments, mirror those found in contemporary pathogenic bacteria. The article argues for the significance of evolutionary history in understanding the adaptation of bacteria, outlining the implications for antibiotic resistance management. By providing insights into evolutionary patterns, this research presents a holistic view of how to address the challenges posed by resistant pathogens effectively.
- https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance – The World Health Organization (WHO) provides a comprehensive overview of antibiotic resistance, detailing its rise as a global health threat exacerbated by the misuse of antibiotics in medicine and agriculture. It discusses how bacteria have developed mechanisms of resistance over time, which complicates treatment strategies. The article emphasizes the need for a multifaceted approach to combat antibiotic resistance, including stewardship programs, improved diagnostics, and public health initiatives. WHO’s insights showcase the urgency of addressing the evolution of resistance mechanisms in the context of healthcare systems worldwide.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
7
Notes:
The narrative discusses recent research (including a 2022 study) and is focused on evergreen science rather than breaking news. While some references are up to date, there is no indication of very recent developments or press releases. Content is not obviously recycled from older articles, but the topic is ongoing and widely covered.
Quotes check
Score:
6
Notes:
The Winston Churchill quote, ‘the longer you can look back, the further you can look forward,’ is not unique to this context and has been widely used elsewhere. The earliest reference to this quote is not found specifically in the provided scientific or medical context, but it is not a recent or original quotation. No other direct quotes from living individuals were found; scientific findings are paraphrased.
Source reliability
Score:
9
Notes:
The narrative references reputable scientific sources (e.g., Nature, ScienceDirect, Cell, WHO, PubMed Central). The Google News link suggests broad syndication, but the original publication or author is not specified. The use of major research journals as references significantly bolsters credibility.
Plausability check
Score:
9
Notes:
The claims about the history and evolution of antibiotic resistance are well-supported by scientific studies and are considered highly plausible within the scientific community. No evidence contradicts the basic assertions, though some details may be contestable depending on the literature reviewed.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative provides a well-grounded, scientifically supported overview of the evolution of antibiotic resistance. It draws on reputable sources and up-to-date research, and the core claims are highly plausible. The Churchill quote is not original, but this does not undermine the scientific content. Overall, the quality and reliability of the information are strong.