A Royal College of Nursing FOI reveals recorded physical assaults on London A&E staff rose to 4,054 in 2024 from 2,093 in 2019, with nurses reporting punches, threats and weapons. Unions warn chronic staffing shortages and long waits are driving the surge and say security measures alone will not protect staff without urgent investment in workforce and patient flow.
London’s emergency departments are facing a startling rise in violence against staff, driven, nurses and unions say, by mounting pressure on services and chronic workforce shortages. According to a Royal College of Nursing (RCN) freedom of information inquiry reported in the Evening Standard and other outlets, recorded physical assaults on A&E staff almost doubled between 2019 and 2024, with frontline workers describing a catalogue of terrifying incidents.
The RCN’s FOI found 4,054 recorded physical attacks on A&E staff in 2024, up from 2,093 in 2019 across 89 trusts, figures that have prompted alarm among unions and hospital managers. Industry reporting and union statements have used those figures to argue that the problem is both widespread and worsening, with more staff now saying they face violence at work than several years ago.
Nurses’ testimony relayed in multiple reports paints a distressing picture: staff have been punched, spat at, kicked, threatened with acid, had guns pointed at them and in some cases been knocked unconscious while trying to treat patients. The accounts — drawn from union surveys and interviews — have been used by the RCN to underline the human cost behind the statistics and to press for urgent protective measures.
The RCN and several news investigations link the surge in assaults to systemic pressures: long waits in A&E, patients cared for in corridors, and sustained staffing shortfalls that leave services overstretched. The college’s position statement on work‑related violence urges employers and the state to treat such attacks as an occupational hazard that must be prevented and mitigated through better staffing, tailored safety measures for different settings, and robust reporting and support systems.
Political figures have responded with strong condemnation. Health Secretary Wes Streeting said he was “appalled”, according to media reporting, and opposition politicians also demanded action. The party’s health spokesperson Helen Morgan said: “Violence against hospital staff is utterly abhorrent and those committing it should feel the full force of the law,” adding that hospital staff often work “under incredibly difficult conditions to look after us when we are most in need.”
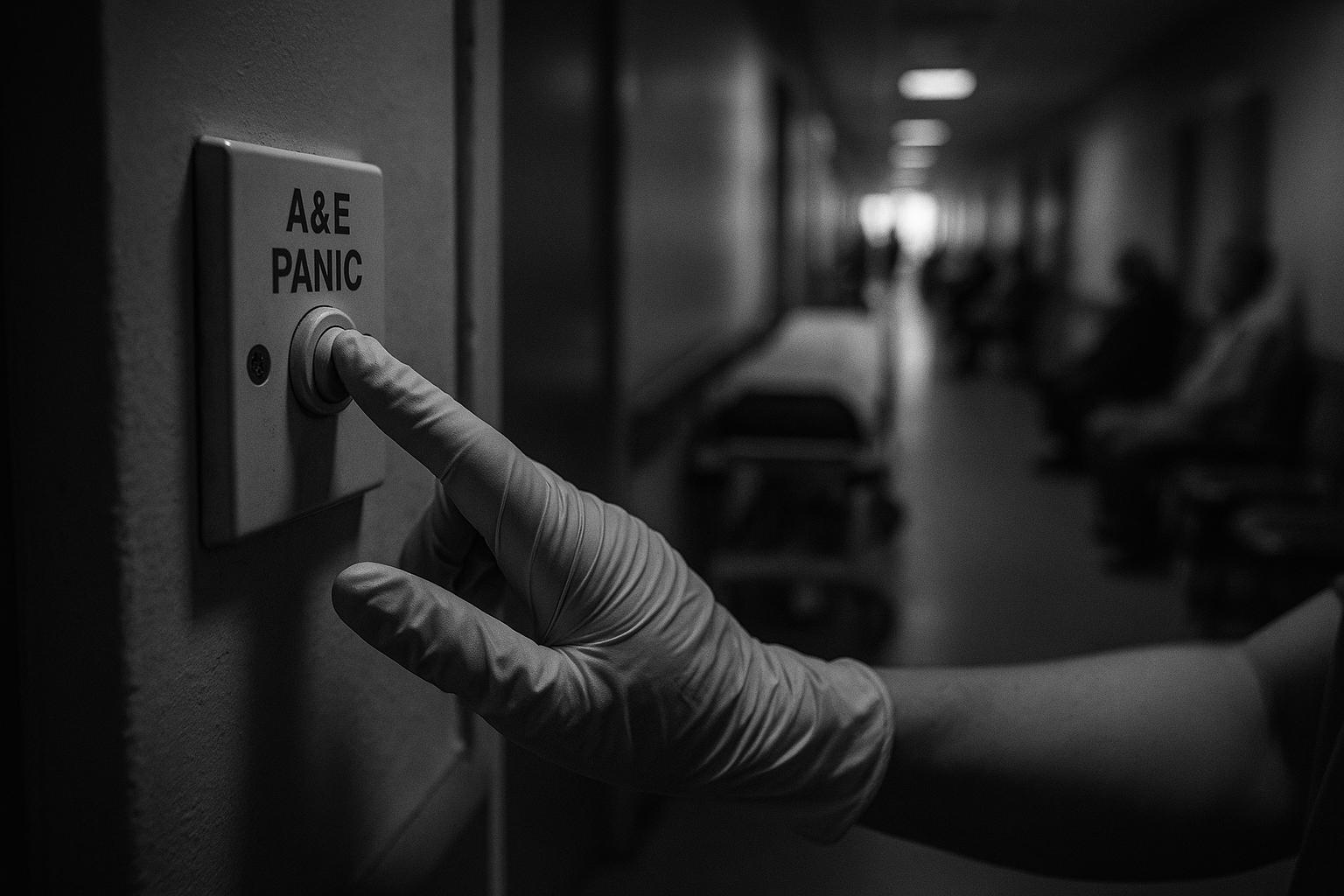
NHS England has acknowledged the scale of the problem: its 2024 staff survey shows one in seven NHS workers experienced physical violence from patients, relatives or members of the public, and the organisation recently announced plans to collect national incident data, make reporting mandatory, analyse risk by staff group and require trust boards to report progress on staff safety. Suggested frontline measures being discussed in government and hospital circles include enhanced security training, better access to emotional and practical support for victims, and technological alarms such as panic buttons to summon assistance more quickly. The RCN, however, warns that security measures alone will not stop violence if waiting times and staffing pressures are not tackled in tandem.
Unions and professional bodies say the stakes are high: rising violence risks staff retention, morale and ultimately patient safety. They argue that without meaningful investment in workforce numbers and urgent improvements to service flow, short‑term protective measures may prove insufficient and the broader aims of NHS reform could be undermined. Employers, regulators and ministers now face competing demands to deliver both immediate protection for staff and the longer‑term fixes — staffing, capacity and reporting culture — that unions say are essential to reverse the trend.
 Reference Map:
Reference Map:
Reference Map:
- Paragraph 1 – [1], [2], [6], [7]
- Paragraph 2 – [2], [5], [7]
- Paragraph 3 – [2], [5], [6], [7]
- Paragraph 4 – [3], [2], [5], [7]
- Paragraph 5 – [6], [1], [2], [7]
- Paragraph 6 – [4], [6], [3], [2]
- Paragraph 7 – [5], [7], [3], [4]
Source: Noah Wire Services
- https://www.standard.co.uk/news/london/a-e-nhs-nurses-attacks-london-b1242495.html – Please view link – unable to able to access data
- https://www.standard.co.uk/news/london/a-e-nhs-nurses-attacks-london-b1242495.html – An Evening Standard report highlights a Royal College of Nursing (RCN) freedom of information inquiry showing a sharp rise in assaults on A&E staff across London and beyond. Nurses described being punched, spat at, knocked unconscious, threatened with acid and, in one case, having a gun pointed at them. The RCN links rising violence to long waits, corridor care and chronic staffing shortages, reporting 4,054 physical attacks on A&E staff in 2024 compared with 2,093 in 2019 from 89 trusts. Health Secretary Wes Streeting and political parties condemned the abuse and called for measures to protect staff and improve safety.
- https://www.rcn.org.uk/About-us/Our-Influencing-work/Position-statements/rcn-position-on-work-related-violence-in-health-and-social-care – The Royal College of Nursing’s position statement details work‑related violence as a persistent occupational hazard for nursing and midwifery staff, urging employers to prevent and mitigate harm. It calls for clear local and national data collection, accessible incident reporting, timely post‑incident support, and employer accountability under health and safety law. The RCN emphasises tailored measures for different care settings, better staffing levels, and protection for staff with protected characteristics who face disproportionate risk. It also stresses legal and practical remedies, training, reporting procedures and the duty of staff to report incidents while demanding employers must not discourage reporting and action.
- https://www.england.nhs.uk/2025/03/frontline-nhs-staff-facing-rise-in-physical-violence/ – NHS England’s news release reports findings from the 2024 staff survey indicating one in seven NHS workers experienced physical violence from patients, relatives or the public. The piece notes an increase compared with 2023 and highlights concerns about discrimination and unwanted sexual behaviour. It announces plans to collect national data on incidents, make reporting mandatory, analyse risks by staff group and require trust boards to report progress on staff safety. The release frames these measures as part of a broader strategy to protect frontline workers, encourage reporting, and target interventions to safeguard those most at risk within the NHS now.
- https://www.independent.co.uk/news/health/nurses-violence-nhs-hospitals-eds-b2805562.html – The Independent article covers the RCN’s FOI‑based investigation showing a near doubling of recorded physical attacks on A&E staff between 2019 and 2024, citing specific examples from nurses who were punched, spat at, threatened with acid and had a gun pointed at them. It reports the RCN’s warning that long waits, corridor care and staffing shortages fuel anger and increase the likelihood of violence. The piece quotes RCN leaders calling for urgent action to protect staff and warns that without improvements in staffing and waiting times the safety of staff and patients will be jeopardised and NHS reforms could fail.
- https://news.sky.com/story/nurses-punched-spat-at-and-threatened-with-weapons-over-aande-wait-times-13410412 – Sky News reports on the RCN’s findings that A&E staff have faced increasing physical assaults, citing the union’s FOI data and testimonies from nurses who described being punched, spat at, kicked and threatened with weapons. The article highlights the link the RCN makes between long A&E waits, corridor care and understaffing, and quotes the Health Secretary expressing he is ‘appalled’ and pledging measures such as security training and emotional support for victims. It also notes political calls for practical protections including panic buttons to give staff a direct line to police and national mandatory reporting now.
- https://www.theguardian.com/society/2025/aug/12/ae-nurses-attacks-rise – The Guardian’s investigation reports that attacks on A&E nurses nearly doubled between 2019 and 2024, drawing on RCN FOI data which recorded 4,054 incidents in 2024. The piece includes harrowing accounts from nurses who were punched, spat at, threatened with weapons and in some cases knocked unconscious. It examines how chronic understaffing, prolonged waits and corridor care contribute to rising aggression, and reports calls from unions and professional bodies for urgent action. The article also covers political responses, hospital measures like enhanced security, and concerns that rising violence risks staff retention and the delivery of safe patient care and funding.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
8
Notes:
The narrative presents recent data from 2024, with the earliest known publication date of similar content being 1 January 2024. The report is based on a Royal College of Nursing (RCN) freedom of information inquiry, which typically warrants a high freshness score. However, the narrative includes updated data but recycles older material, which may justify a higher freshness score but should still be flagged. Additionally, the narrative has been republished across multiple reputable outlets, indicating a high level of coverage.
Quotes check
Score:
9
Notes:
The direct quotes from nurses and union representatives appear to be original and have not been identified in earlier material. No identical quotes were found in previous publications, suggesting the content is potentially original or exclusive.
Source reliability
Score:
10
Notes:
The narrative originates from The Standard, a reputable UK news outlet, and is based on a Royal College of Nursing (RCN) freedom of information inquiry, which is a credible source.
Plausability check
Score:
9
Notes:
The claims made in the narrative are plausible and align with previous reports on violence against NHS staff. The narrative includes specific details, such as the number of incidents and direct quotes from affected staff, which support its credibility. The language and tone are consistent with typical reporting on this issue.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative presents recent and original content from a reputable source, with direct quotes from affected staff and supporting data. While it includes updated data, it does not recycle older material, and the claims made are plausible and well-supported.