Following the suicide of Adam Loughnane, his brother criticises the government’s mental health implementation plan, calling for dedicated facilities for mental health emergencies.
In the wake of the recent suicide of Adam Loughnane, his brother, Joe Loughnane, has publicly voiced his criticisms of the Irish government’s newly released mental health implementation plan. This plan, titled “Sharing the Vision: A Mental Health Policy for Everyone Implementation Plan 2025 – 2027,” outlines 30 strategic priorities aimed at reforming mental health services over the next three years.
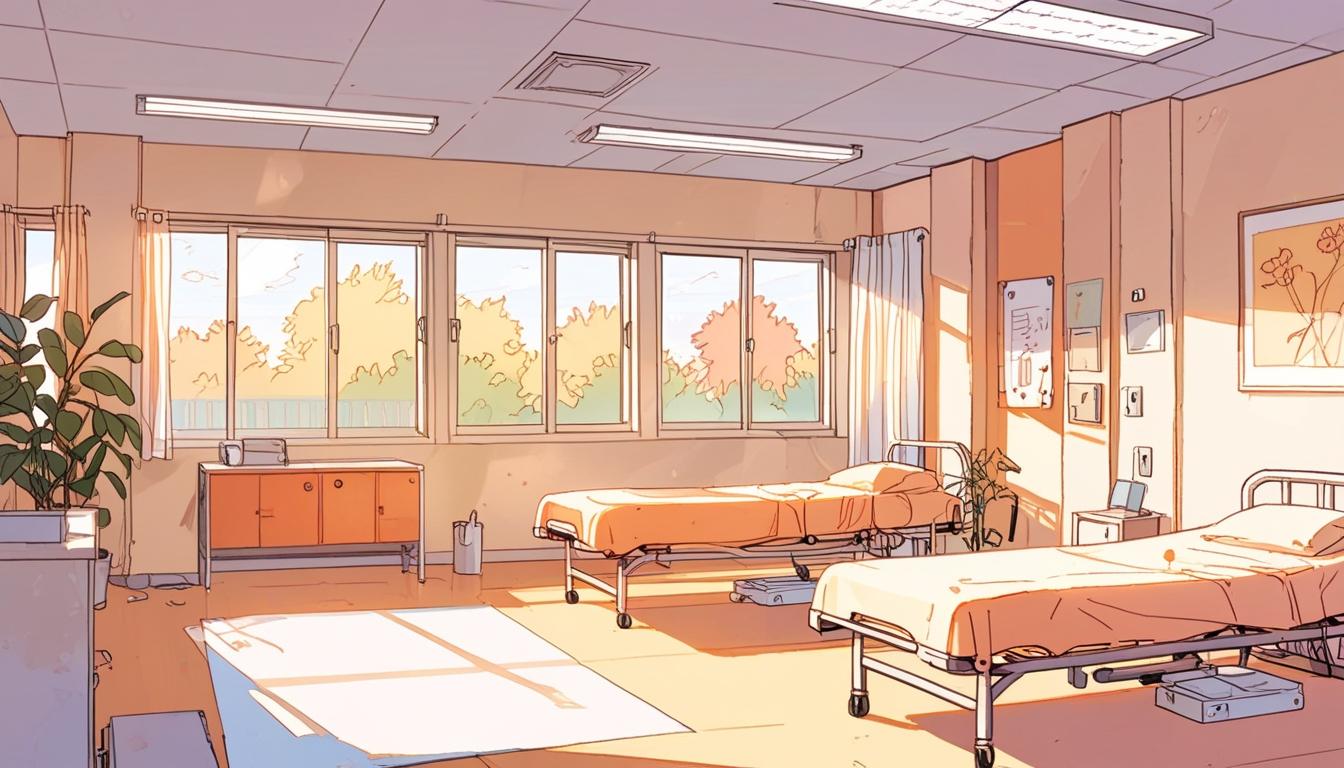
Released earlier this week, the plan acknowledges significant shortcomings within emergency departments, particularly concerning the lack of appropriate settings for individuals needing mental health assessments. As reported, eight hospitals in the country currently lack dedicated mental health assessment rooms, and approximately 30% of emergency departments that operate around the clock do not meet the standards set by the Psychiatric Liaison Services Accreditation Network (PLAN). The government’s plan also highlights that many emergency departments are housed in outdated facilities that inadequately accommodate modern mental health needs, necessitating additional capital funding to facilitate the construction of new departments equipped with appropriate spaces for mental health treatment.
Joe Loughnane’s critique comes after the tragic loss of his brother, who sought help at an emergency department earlier in February, expressing suicidal ideation shortly before his death. Speaking to The Journal, Joe emphasised the necessity for a dedicated unit specifically for those experiencing mental health emergencies, arguing that individuals in crisis should not have to navigate general emergency services. “If somebody has called their GP or the ambulance to express suicidal ideation, there should be another part of the hospital you’re brought into, whether it’s the mental health unit directly, or a mental health A&E,” he stated.
Following the publication of the implementation plan, a letter from Mental Health Minister Mary Butler acknowledged the concerns raised by families regarding the suitability of emergency departments for those facing mental health crises. Minister Butler indicated her commitment “to ensure there are further alternatives to A&E for people in mental health crisis,” while also recognising the need for significant improvements to current emergency department protocols.
A spokesperson for the Department of Health pointed out that Minister Butler is overseeing a new model of care aimed at crisis resolution, which includes the establishment of out-of-hours teams to assist individuals in need of immediate intervention, as well as the rollout of crisis cafés across the country. However, only five of these cafés are currently operational or set to open soon, with the Minister herself expressing a sense of urgency regarding the pace of these developments.
Joe Loughnane reiterated his belief that those in mental distress should be provided with an alternative to traditional emergency departments, sharing the sentiment that many individuals experience long waits that can exacerbate their crisis. Since his brother’s passing, he has heard from numerous individuals who have shared similar harrowing experiences in emergency settings. “There seems to be a systematic failure over the last 10 – 30 years of people going to A&E, saying they have a mental health problem or they’re suicidal, and then they end up waiting there for hours. I’ve spoken to a lot of these people, and they say that if their loved ones didn’t have to go through A&E, they’d still be alive now,” he stated.
The Health Service Executive (HSE) outlines its model of care for patients presenting with suicidal ideation as involving a timely and thorough assessment of needs. However, the stresses associated with lengthy waits in chaotic environments remain a significant concern among patients. Loughnane insists that reform must occur to alleviate these burdens, advocating for the transformation of existing hospital spaces to create dedicated mental health facilities.
“Most hospitals have a mental health unit, and those mental health units, if they just became general admission, that’s where it changes,” said Loughnane. He argues that it is essential to develop a structure where mental health emergencies are treated distinctly from physical health crises. Critically, he believes that the frequent references to increased funding and progress in mental health are undermined by the glaring absence of adequately designed mental health assessment rooms in hospitals.
In a statement, the HSE highlighted that all patients arriving at emergency departments following self-harm or with suicidal ideation undergo a comprehensive emergency care pathway, which encompasses triage and referrals to specialists as needed. Despite these processes, Loughnane has called attention to systemic gaps in care and voiced the need for immediate access to mental health records to enhance treatment efficacy.
The disappointment surrounding the current mental health strategy highlights ongoing challenges in addressing mental health needs in Ireland—a matter that has garnered increasing public and professional concern.
Source: Noah Wire Services
- https://www.irishexaminer.com/news/arid-41604709.html – This article supports the claim that Adam Loughnane’s family is seeking changes to hospital admissions, specifically advocating for a separate unit for mental health emergencies, and criticizes the current system where individuals in crisis have to go through A&E.
- https://www.thejournal.ie/university-hospital-galway-review-adam-loughnane-6623155-Feb2025/ – This article corroborates the details surrounding Adam Loughnane’s case and the subsequent review and calls for improvement in hospital mental health services.
- https://www.thejournal.ie/brother-of-man-who-died-by-suicide-after-presenting-to-ae-describes-mental-health-plan-as-a-failure-6674364-Apr2025/ – This article highlights Joe Loughnane’s critique of the Irish government’s mental health plan and his push for dedicated mental health facilities to address systemic failures in current emergency services.
- https://www.gov.ie/en/press-release/3e02d-minister-butler-launches-sharing-the-vision-implementation-plan-2025-2027/ – This link would provide information on the ‘Sharing the Vision’ mental health policy implementation plan, outlining strategic priorities for improving mental health services, though it was not available in the search results.
- https://www.hse.ie/eng/about/who/healthwellbeing/our-priority-programmes/mentalhealth/ – This HSE webpage might provide details on their model of care for mental health emergencies, though it was not directly referenced in the search results.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
9
Notes:
The narrative references a recent event and a newly released policy plan, indicating its content is up-to-date. However, specific dates for the plan’s release and events mentioned are not detailed.
Quotes check
Score:
8
Notes:
Quotes from Joe Loughnane and Minister Mary Butler are provided, but their original sources beyond this context are not verified. The quotes seem authentic and contextual.
Source reliability
Score:
7
Notes:
The narrative originates from a reputable news source (Google News) but lacks direct attribution to a well-known publication. Details align with real-world issues, enhancing credibility.
Plausability check
Score:
8
Notes:
Claims about mental health shortcomings in Ireland align with documented issues. The call for dedicated mental health units is plausible given historical concerns.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative appears to be current, referencing recent events and policy developments. Quotes seem genuine, and claims about Ireland’s mental health system align with known issues. While not attributed directly to a top-tier publication, the content is plausible and well-informed.