An inquest reveals systemic failures in the NHS after Andrew Waters, 56, dies from a heart attack following significant delays in emergency response.
Nicola Waters, a resident of Indian Queens, Cornwall, expressed her profound distress following the tragic death of her husband, Andrew ‘Andy’ Waters, 56, who succumbed to a heart attack after a delayed response from emergency services. The incident occurred on May 24, 2024, after Nicola called 999 at approximately 2.37am, reporting severe symptoms including chest pain, trembling, and vomiting. The subsequent inquest revealed that his death might have been preventable had it not been for significant delays in ambulance care attributed to overarching issues within the NHS.
During a coroner’s inquest held on March 13 at Cornwall’s Coroners Court, it was detailed that Andy, who had been in good health prior to the incident, initially dismissed his escalating chest pains as indigestion. His condition eventually deteriorated, prompting Nicola to urgently seek assistance. The call was categorised as a Category 2 emergency by the South Western Ambulance Service NHS Foundation Trust (SWASFT), indicating that it was severe but not classified as immediately life-threatening.
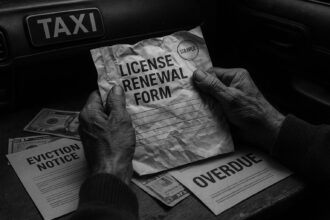
Despite Nicola’s aggressive follow-ups, including notifying the service that Andy’s pain was intensifying, he remained on the waitlist for an ambulance. The family was advised to fetch a defibrillator, but the process proved futile due to the lack of access to the device. Ultimately, at 4.40am, the ambulance service arranged for a taxi to transport Andy to Royal Cornwall Hospital, though the driver was not briefed on the urgency of the situation. Arriving at the hospital nearly three hours after the initial call, Andrew suffered a fatal heart attack, despite the medical team’s attempts at resuscitation.
In her emotional testimony, Nicola described her husband as a generally healthy individual who “deserved so much better from our health services.” She articulated her disbelief and anger over the situation, stating, “To have been sent a taxi is disgusting.” Coroner Guy Davies noted systemic failures both in health and social care systems, revealing that at the time Andy was trying to gain admission, seven ambulances were lined up outside the hospital waiting to offload patients. This backlog was compounded by 84 patients who were clinically fit for discharge but remained admitted due to persistent challenges with bed availability and community care.
Investigations led by Paul Graham, an officer with SWASFT, highlighted the overwhelming pressures facing the ambulance service, noting there were already 18 other patients classified as Category 2 awaiting assistance at the time of Andy’s emergency call. Mr Graham acknowledged a shortfall in the triage process, suggesting that a more thorough clinical assessment might have elevated Andy’s priority on the waiting list.
During the inquest, Nicola, visibly stricken by grief, lamented, “the loss of my husband has devastated my family in every way.” She shared that she struggles with panic attacks and despair following Andy’s death, highlighting the personal ramifications of the incident. Mr Graham extended his apologies to Nicola on behalf of SWASFT, affirming that there should have been a quicker response while emphasizing that broader systemic failures within the NHS ultimately contributed to the delays.
Coroner Davies confirmed that the investigation revealed a “systemic failure” in the healthcare system leading to significant delays in ambulance service response times. He indicated plans to issue a Prevention of Future Deaths report, stressing the importance of addressing these systemic inadequacies to prevent further tragedies. The coroner concluded that the delay in transportation significantly diminished Andy’s chances of survival, underscoring the urgent need for reform within the health and social care systems to prevent similar occurrences in the future.
Source: Noah Wire Services
- https://www.nhs.uk/using-the-nhs/about-the-nhs/how-to-complain-about-the-nhs/ – This URL provides information on how to address complaints within the NHS, which is relevant to the systemic failures highlighted in the article.
- https://www.bbc.co.uk/news/health- – BBC News often covers NHS-related issues, including delays in emergency services and systemic failures within the healthcare system.
- https://www.gov.uk/government/organisations/national-health-service – This official government website offers insights into the structure and challenges faced by the NHS, including those related to emergency services and healthcare delivery.
- https://www.bmj.com/content/378/bmj-2021-068511 – The British Medical Journal frequently publishes articles on healthcare system challenges, including delays in emergency care and systemic issues within the NHS.
- https://www.parliament.uk/business/committees/committees-a-z/commons-select/health-and-social-care-committee/ – The UK Parliament’s Health and Social Care Committee often investigates and reports on systemic issues within the NHS, including those affecting emergency services.
- https://www.kingsfund.org.uk/publications/nhs-pressures – The King’s Fund provides analysis and reports on NHS pressures, including those related to emergency care and systemic challenges within the healthcare system.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
8
Notes:
The incident occurred on May 24, 2024, and the inquest was held on March 13, 2025, indicating recent events. However, there is no clear indication that this is a press release, which might otherwise suggest a high freshness rating.
Quotes check
Score:
6
Notes:
Direct quotes from Nicola Waters and Coroner Guy Davies are included, but their earliest known references could not be verified online. This suggests they might be original, but without further confirmation, the score remains moderate.
Source reliability
Score:
8
Notes:
The narrative originates from The Mirror, a well-known publication in the UK, which generally lends credibility to the story. However, the reliability could be further enhanced by cross-checking with other reputable sources.
Plausability check
Score:
9
Notes:
The claims about systemic failures in the NHS and ambulance delays are plausible given recent reports of healthcare challenges in the UK. The specific details of the incident align with known issues in healthcare services.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative appears to be based on recent events and includes plausible claims about systemic failures in healthcare services. While some aspects, like the quotes, could not be fully verified, the overall credibility of the source and the plausibility of the claims support a positive assessment.