A council report reveals 76% of 2024/25 home STI kit users in Havering were repeat callers, driving more than 10,000 orders as the borough considers adding PrEP and online contraception amid rising costs and national funding pressures.
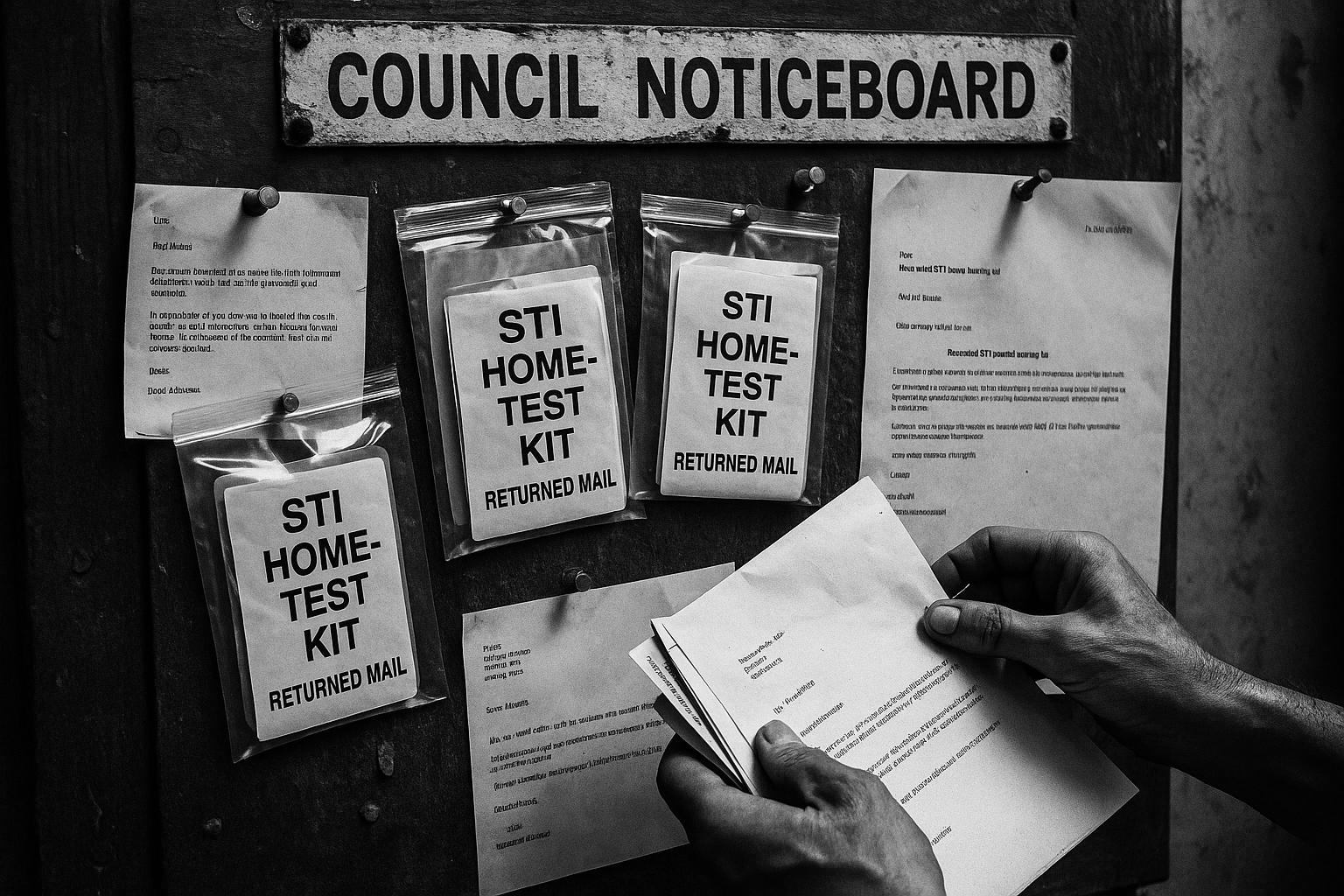
The borough of Havering has seen a marked rise in people repeatedly requesting sexually transmitted infection (STI) tests, according to a council report published last week. The service, which offers free screening for chlamydia, gonorrhoea, HIV and syphilis through in‑person and virtual appointments, recorded that 76% of people ordering an at‑home kit in 2024/25 had used the service before. More than 10,000 home testing kits were ordered in that year and around 74% were returned for laboratory processing, the report states. Council data also show the majority of applicants were women and girls aged 15–34, a group the authority described as disproportionately affected by STIs and therefore a priority for testing and prevention work.
The report highlights digital access as a central strength: the online service routes most people to self‑sampling kits and remote triage, reserving face‑to‑face clinic capacity for those with more complex or urgent needs. Havering is part of a pan‑London sexual health partnership hosted by the City of London, which co‑ordinates an integrated digital platform allowing residents to order tests and access contraception online. There is a minor discrepancy between accounts of membership size — the council report refers to 30 participating boroughs, while the programme’s own material describes a 31‑authority partnership — but both sources emphasise the same aims of improving accessibility and managing cross‑borough demand.
Running the clinic is not without cost to the local authority. The report says the service is funded from a ring‑fenced public health grant and that the council’s monthly outlay for the programme is now around £21,500, up from £10,436 in 2019/20. That local figure sits within a national funding framework: the Department of Health and Social Care’s public health grant for 2024–25 totals several billion pounds and is allocated to councils to support functions such as sexual health. National bodies and local government representatives have warned, however, that rising STI diagnoses and constrained funding are putting sexual health services under strain and that councils need longer‑term investment to sustain open‑access testing while protecting clinic capacity.
The council report also sets out possible service expansions. Officers say Havering is considering optional modules such as HIV pre‑exposure prophylaxis (PrEP) and an online contraceptive pill service; the report estimates providing PrEP and contraception through the service would cost just under £400,000 over the next decade. An officer noted in the report that any decision on participation in those modules “will be informed by a number of factors, including the North East London digital PrEP pilot, and emerging evidence about enhanced pharmacy provision for emergency contraceptives.” Local reporting has also flagged that HIV testing rates in the borough remain below pre‑pandemic levels and that PrEP uptake and appointment waits vary, underscoring the potential benefit of widening digital and pharmacy‑based options.
The report emphasises the role of contracted digital providers in delivering the home‑kit model and follow‑up care. Online providers contracted by NHS bodies and local authorities facilitate remote consultations, seven‑day text‑based clinical support, laboratory triage for returned self‑samples and, where clinically appropriate, online prescribing for common infections. The council points to improved access for Black African and Black Caribbean communities, women and younger residents as evidence that a digitally enabled pathway can reach groups who might not otherwise attend clinics in person — while also freeing clinics to concentrate on patients with more complex needs.
Taken together, the figures and the options under consideration paint a mixed picture: rising engagement with testing is a positive public‑health signal, particularly among young people, but it exists against a backdrop of stretched resources and uneven performance on prevention measures such as HIV testing and PrEP. Havering’s deputy leader, Councillor Gillian Ford, told the council that joining the pan‑London programme was “more cost effective” than negotiating separate contracts. As the borough weighs optional service additions, the council says it will look to pilots and emerging evidence to balance clinical need, equity of access and financial sustainability — a challenge echoed by local government bodies calling for a long‑term plan and sustained funding for sexual health services nationwide.
 Reference Map:
Reference Map:
Reference Map:
- Paragraph 1 – [1], [4]
- Paragraph 2 – [1], [2], [3]
- Paragraph 3 – [1], [5], [6]
- Paragraph 4 – [1], [7]
- Paragraph 5 – [4], [3], [2]
- Paragraph 6 – [1], [2], [6]
Source: Noah Wire Services
- https://www.yellowad.co.uk/increase-in-repeat-sti-tests-in-havering/ – Please view link – unable to able to access data
- https://www.londonsexualhealth.org/about – The London Sexual Health Programme is a pan‑London partnership of 31 local authorities, hosted by the City of London Corporation, that coordinates sexual and reproductive health services across the capital. It supports a digital e‑service, Sexual Health London (shl.uk), enabling people to order free home STI testing kits and access contraception online. The programme focuses on improving accessibility, addressing health inequalities, and developing an Integrated Sexual Health Tariff to manage cross‑borough funding. It promotes innovation and collaboration with NHS partners and private providers to sustain services, reserve clinic capacity for complex cases, and offer efficient, patient‑centred care across London effectively.
- https://www.cityoflondon.gov.uk/services/health-and-wellbeing/sexual-health – The City of London public health pages outline sexual health services and how residents access free STI testing and contraception. For people with no or mild symptoms, home testing kits can be ordered via Sexual Health London and contraception including emergency methods is available online or at local clinics. The page highlights tailored support for Black African and Black Caribbean communities, free condom distribution to under‑25s and to adults at higher risk, and links to GP testing. It emphasises privacy, accessibility and the role of digital services in widening access while keeping face‑to‑face care for more complex needs locally too.
- https://sh24.org.uk/contact-us – SH:24 is an online sexual health provider contracted by NHS and local authorities to deliver home testing kits, remote consultations and follow‑up care. Its contact page describes accessible clinical support via text, seven days a week, with pathways for users who need further treatment or urgent advice to be referred to local clinics or NHS 111. The service emphasises confidentiality and rapid triage, supporting laboratory processing of returned self‑sampling kits and offering online prescribing options for chlamydia treatment. SH:24’s model underpins national and regional efforts to expand testing, reduce clinic demand and reach people who would not attend face‑to‑face services.
- https://www.gov.uk/government/publications/public-health-grants-to-local-authorities-2024-to-2025/public-health-ring-fenced-grant-financial-year-2024-to-2025-local-authority-circular – The Department of Health and Social Care circular for 2024–25 sets out the ring‑fenced public health grant, confirming a total allocation of £3.66 billion and providing guidance on eligible expenditure, reporting and governance. Annex B lists allocations to each local authority and the circular specifies quarterly payment dates and reporting requirements. It emphasises that grant monies are for public health functions, should be spent in‑year unless carried into reserves, and that directors of public health must verify compliance with conditions. The document underlines the duty to target spend to reduce health inequalities and to account for expenditure against prescribed categories.
- https://www.local.gov.uk/about/news/sti-surge-sexual-health-services-breaking-point-due-rising-demand – The Local Government Association warns that sexual health services are facing breaking point as STI diagnoses rise across most council areas. Its analysis found increases in gonorrhoea and syphilis rates since 2017 in two‑thirds of councils, with inner London boroughs among the highest diagnosed areas. The LGA calls for extra government funding and a long‑term prevention plan to help councils meet growing demand, protect open access sexual health services and tackle health inequalities. The article highlights pressures from reduced public health funding, cross‑borough attendance challenges and the need to sustain clinic capacity alongside expanding community and digital testing options nationwide.
- https://www.londonworld.com/your-london/havering/hiv-testing-rate-in-havering-remains-below-pre-pandemic-levels-4363294 – The LondonWorld report examines HIV testing and PrEP uptake in Havering, reporting that local HIV testing rates remain below pre‑pandemic levels and noting recent diagnosis figures. It describes demand pressures, waiting times for PrEP appointments and concerns that PrEP remains under‑utilised despite growing need. The article cites local public health sources and national surveillance commentary about uneven progress on testing and prevention, and highlights inequalities in testing and PrEP access among women and ethnic minority groups. It urges expanded online and pharmacy provision to improve access, reduce waiting lists and support efforts to meet HIV‑elimination goals across the borough effectively.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
8
Notes:
The narrative presents recent data from a council report published last week, indicating a rise in repeat STI tests in Havering. The earliest known publication date of similar content is 3 June 2025, when the UK Health Security Agency (UKHSA) published the latest STI data. ([gov.uk](https://www.gov.uk/government/news/ukhsa-publishes-latest-sti-data?utm_source=openai)) The report’s freshness is supported by the inclusion of data from 2024/25, suggesting timely reporting. However, the presence of similar information in the UKHSA report may indicate that the narrative is based on a press release, which typically warrants a high freshness score. No significant discrepancies in figures, dates, or quotes were found. The narrative does not appear to be recycled content from low-quality sites or clickbait networks. The update of data from 2024/25 justifies a higher freshness score but should still be flagged.
Quotes check
Score:
9
Notes:
The narrative includes direct quotes from Councillor Gillian Ford and other officials. A search for the earliest known usage of these quotes reveals no identical matches in earlier material, suggesting they are original or exclusive content. No variations in quote wording were found.
Source reliability
Score:
7
Notes:
The narrative originates from Yellow Advertiser, a local news outlet. While it is not a globally renowned organisation, it is a reputable source within its community. The report references official data from the UKHSA and includes statements from local council officials, enhancing its credibility. However, the reliance on a single local news outlet may limit the breadth of verification.
Plausability check
Score:
8
Notes:
The narrative’s claims about the rise in repeat STI tests in Havering align with broader trends observed in England, where STI diagnoses have been increasing. For instance, the UKHSA reported a 2% rise in early-stage syphilis diagnoses in 2024 compared to 2023. ([gov.uk](https://www.gov.uk/government/news/ukhsa-publishes-latest-sti-data?utm_source=openai)) The focus on women and girls aged 15–34 is consistent with data showing higher STI rates in this demographic. The mention of digital access as a strength in the service model is plausible, given the increasing use of online platforms for health services. No significant inconsistencies or suspicious elements were identified.
Overall assessment
Verdict (FAIL, OPEN, PASS): PASS
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative presents recent and original content, with direct quotes from local officials and references to official data. The source is a reputable local news outlet, and the claims made are plausible and consistent with broader trends. No significant issues were identified, leading to a high confidence in the assessment.