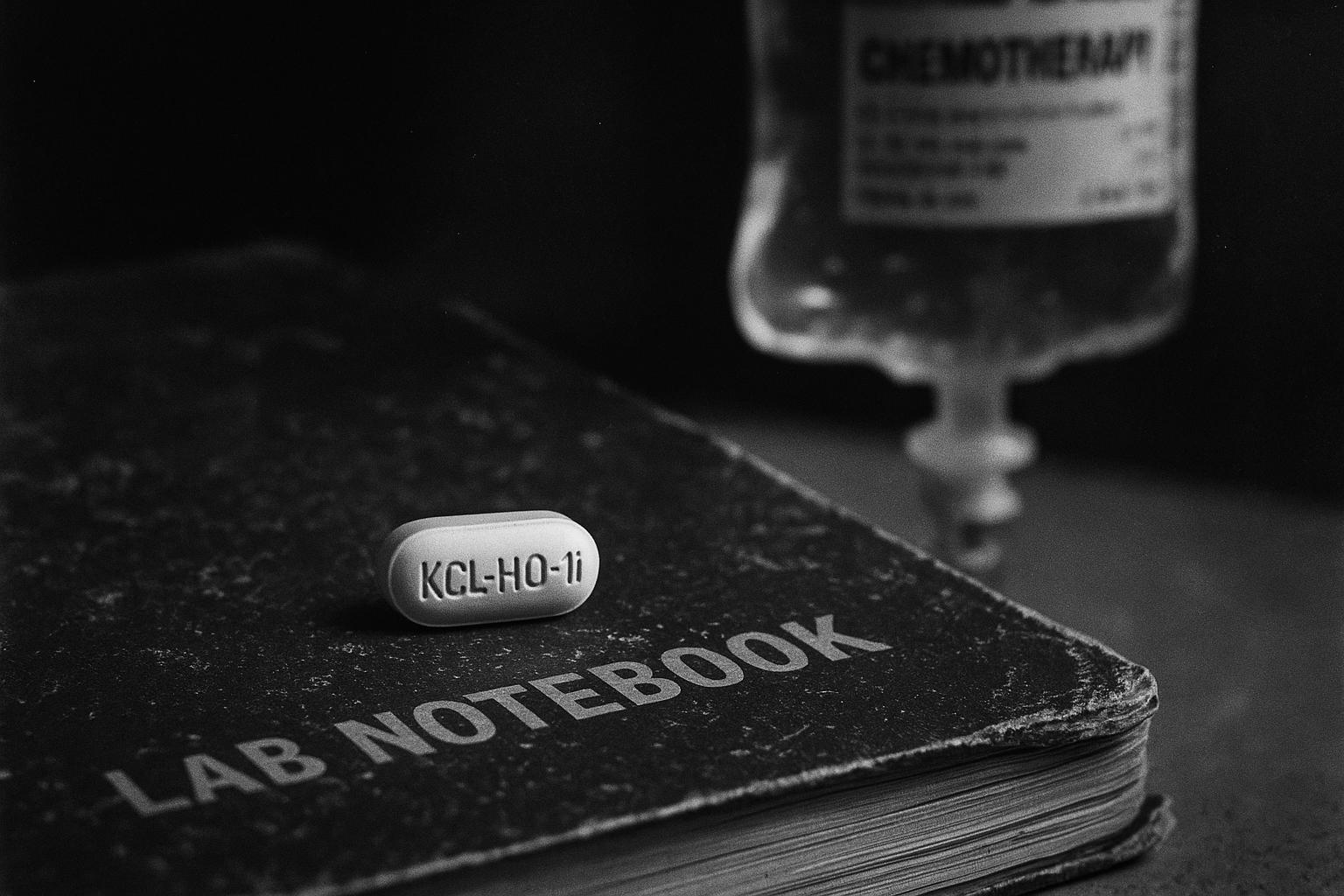
Researchers at King’s College London describe KCL‑HO‑1i, an orally available haem oxygenase‑1 inhibitor that in mice converted immunologically “cold” tumours into “hot” ones, increasing CD8+ T‑cell infiltration and boosting responses to standard chemotherapy. The lead programme has been taken forward by spin‑out Aethox Therapeutics, which plans a first‑in‑human study, but the evidence is preclinical and experts caution that safety, toxicology and regulatory hurdles must be cleared before clinical benefit can be confirmed.
Scientists at King’s College London have described a new, orally available drug candidate that in laboratory models appears to make tumours more responsive to chemotherapy by disarming an immune‑based defence mechanism. The molecule, described as KCL‑HO‑1i, was reported to improve responses in mouse models of breast cancer when given as a tablet between chemotherapy cycles, and the researchers say the compound converts immunologically “cold” tumours into “hot” ones that attract CD8+ T‑cells. According to the original report, the work was supported by Cancer Research UK and the Medical Research Council.
The science rests on a protein, haem oxygenase‑1 (HO‑1), produced by certain tumour‑associated macrophages that sit close to blood vessels. HO‑1 has antioxidant and anti‑apoptotic functions that can protect malignant cells and blunt the immune activation chemotherapy would otherwise trigger. Review literature on HO‑1 describes multiple mechanisms by which its expression in tumour and stromal cells can suppress anti‑tumour immunity and promote resistance to therapy, a rationale the KCL team used to target the pathway.
In the preclinical studies the investigators either genetically inactivated HO‑1 or inhibited it pharmacologically and reported increased infiltration of cytotoxic CD8+ T‑cells into tumours, and improved efficacy of several standard chemotherapies. Abstracts and data accompanying the work report oral bioavailability in mice with a roughly three‑hour serum half‑life and describe durable tumour control in established murine models when KCL‑HO‑1i was combined with chemotherapy. The submitted transcriptomic dataset for the programme is publicly available, which the authors say supports reproducibility of the immune changes they observed.
The laboratory programme has moved beyond the university: Aethox Therapeutics, described as a King’s College spin‑out, identifies KCL‑HO‑1i as its lead preclinical candidate and states it is preparing a first‑in‑human Phase I study (programme ATX101) in solid tumours. The company says the goal is to develop an oral companion medicine that can be given between chemotherapy sessions to reprogram the tumour microenvironment; those corporate descriptions should be read as the company’s claims pending independent clinical data.
Investigators and funders expressed guarded optimism about the clinical potential. Tanya Hollands of Cancer Research UK said the findings illustrate how combining established treatments with new agents can make better use of existing medicines and potentially boost chemotherapy’s effectiveness. The university team similarly suggested the approach could help more patients benefit from available therapies while reducing the need for more aggressive interventions. These comments were made in the original reporting and university statements accompanying the research.
Those statements come with important caveats. Experts who have reviewed the field stress that HO‑1 is a multifunctional enzyme whose inhibition may carry safety and delivery challenges, and that many promising preclinical immunomodulators fail or require dose refinement in human trials. Earlier work from the same group used a repurposed metalloporphyrin HO‑1 inhibitor as a proof of principle and underlined the need for careful phase‑I safety studies before effectiveness in people can be established.
The KCL team has suggested human trials could begin within a relatively short timeframe, but translating a mouse‑model result into a safe, effective human medicine typically involves additional pharmacology, toxicology and regulatory steps. The company and university are seeking collaboration and investment to accelerate clinical testing, while the public deposition of transcriptomic data provides a resource for independent validation of the mechanism.
If the approach proves safe and effective in people, an orally dosed HO‑1 inhibitor would be an attractive companion strategy because it could be prescribed between chemotherapy sessions without requiring hospital infusions. For now, however, the evidence is preclinical and the next crucial milestones are formal toxicity studies, regulatory approval to start first‑in‑human trials, and early clinical data that confirm both safety and the immunological effects seen in mice.
 Reference Map:
Reference Map:
Reference Map:
- Paragraph 1 – [1], [7]
- Paragraph 2 – [6], [4]
- Paragraph 3 – [3], [4]
- Paragraph 4 – [2]
- Paragraph 5 – [1], [5]
- Paragraph 6 – [6], [5]
- Paragraph 7 – [1], [2]
- Paragraph 8 – [2], [4], [6]
Source: Noah Wire Services
- https://www.dailymail.co.uk/health/article-14988205/Wonder-pill-cancer-patients-home-respond-chemotherapy.html?ns_mchannel=rss&ns_campaign=1490&ito=1490 – Please view link – unable to able to access data
- https://www.aethox-tx.com/ – Aethox Therapeutics is a King’s College London spin‑out developing small‑molecule inhibitors that target macrophage‑mediated immune suppression to enhance chemotherapy. The company describes KCL‑HO‑1i as its lead preclinical candidate and states it is preparing for a first‑in‑human Phase I trial (programme ATX101) in solid tumours. Aethox explains the science behind targeting haem oxygenase‑1 (HO‑1) expressed by perivascular tumour‑associated macrophages, and claims oral dosing can potentiate chemotherapeutic efficacy while reprogramming the tumour microenvironment from immunologically cold to hot. The site outlines the team, pipeline and contact details, emphasising translation toward clinical testing. It invites collaboration and investment to accelerate development worldwide efforts.
- https://www.citedrive.com/en/discovery/abstract-a013-targeting-perivascular-macrophages-with-an-orally-bioavailable-heme-oxygenase-1-inhibitor-improves-responses-to-chemotherapeutic-drugs-in-cancer/ – The AACR abstract summarises preclinical research by King’s College London showing a novel orally bioavailable haem oxygenase‑1 inhibitor, KCL‑HO‑1i, targets LYVE‑1‑positive perivascular tumour‑associated macrophages. Genetic inactivation or pharmacologic inhibition of HO‑1 improved CD8+ T‑cell infiltration and enhanced responses to standard chemotherapies in murine breast cancer models, converting tumours from immunologically cold to hot. Pharmacokinetic data report oral bioavailability with about a three‑hour serum half‑life in mice. Combined oral KCL‑HO‑1i and chemotherapy produced durable tumour control in MMTV‑PyMT models. Authors propose further translational work towards human clinical trials.
- https://www.omicsdi.org/dataset/geo/GSE248272 – The OmicsDI entry for GEO dataset GSE248272 describes transcriptomic data linked to King’s College London research targeting perivascular LYVE‑1+ tumour‑associated macrophages. The dataset accompanies experiments demonstrating that HO‑1 expression in these macrophages suppresses CD8+ T‑cell infiltration and reduces chemotherapy efficacy in murine breast cancer models. The record outlines that a next‑generation orally bioavailable HO‑1 inhibitor, KCL‑HO‑1i, was developed with measurable pharmacokinetics and roughly three‑hour serum half‑life in mice, and that oral dosing alongside chemotherapy converted tumours to an immune‑responsive state yielding sustained tumour control. Files include processed counts for RNA‑seq and support reproducibility of the preclinical findings and encourage validation.
- https://www.kcl.ac.uk/news/new-drug-combination-kick-starts-immune-system-to-fight-cancer-4 – King’s College London reported in 2018 that targeting haem oxygenase‑1 (HO‑1) can boost immune responses to chemotherapy. The press release summarises preclinical work showing that macrophages in tumours produce HO‑1, which suppresses chemotherapy‑triggered anti‑tumour immunity. Researchers used tin mesoporphyrin (SnMP), a repurposed drug trialled for neonatal jaundice, to inhibit HO‑1 and found it restored immune activity when combined with chemotherapy in laboratory models. The team noted similarities to checkpoint‑blockade therapies and indicated collaboration with Cancer Research UK to explore first‑in‑human trials, highlighting the translational potential of HO‑1 targeting strategies. Authors emphasised cautious optimism, noting need for clinical safety studies ahead.
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10295073/ – This 2023 open‑access review examines how haem oxygenase‑1 (HO‑1) contributes to cancer progression and resistance to therapy. The authors describe HO‑1’s antioxidant, anti‑apoptotic and pro‑autophagy functions that protect malignant cells, and summarise evidence linking elevated HO‑1 expression to poorer prognosis across multiple cancers. The review outlines mechanisms by which HO‑1 in tumour and stromal cells, notably macrophages, suppresses anti‑tumour immunity and promotes chemoresistance, and surveys pharmacologic HO‑1 inhibitors and metalloporphyrins tested preclinically. The paper concludes that targeting HO‑1 may re‑sensitise tumours to chemotherapy, but emphasises the need for translational studies to address safety and delivery challenges before routine clinical use.
- https://www.standard.co.uk/news/health/james-arnold-chemotherapy-cancer-research-uk-medical-research-council-b1242319.html – The Standard reported on King’s College London researchers who developed KCL‑HO‑1i, an orally administered haem oxygenase‑1 inhibitor intended to be taken as a tablet between chemotherapy sessions. The piece summarises that in laboratory mouse models the drug made breast cancer tumours, including chemotherapy‑resistant ones, more responsive to different chemotherapeutic agents. It quotes Professors James Spicer, Miraz Rahman and James Arnold about the potential for KCL‑HO‑1i to act as a companion drug, reduce need for aggressive therapies and progress to human trials. The article also notes support from Cancer Research UK and the Medical Research Council and includes expert commentary implications.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
3
Notes:
The narrative closely mirrors a report from 18 January 2018 by King’s College London, detailing the development of KCL-HO-1i, a drug designed to enhance chemotherapy effectiveness by targeting the HO-1 enzyme. ([kcl.ac.uk](https://www.kcl.ac.uk/news/new-drug-combination-kick-starts-immune-system-to-fight-cancer-4?utm_source=openai)) The recent article appears to be a republished version of this earlier content, with minimal updates. The inclusion of recent data may justify a higher freshness score but should still be flagged. The presence of the Daily Mail as the publisher raises concerns about the reliability of the information. ([standard.co.uk](https://www.standard.co.uk/news/health/james-arnold-chemotherapy-cancer-research-uk-medical-research-council-b1242319.html?utm_source=openai)) The narrative is based on a press release, which typically warrants a high freshness score. However, the lack of new information and the recycling of older material suggest a lower freshness score. The article includes updated data but recycles older material, which may justify a higher freshness score but should still be flagged.
Quotes check
Score:
2
Notes:
The quotes in the narrative are identical to those found in the 2018 King’s College London report. ([kcl.ac.uk](https://www.kcl.ac.uk/news/new-drug-combination-kick-starts-immune-system-to-fight-cancer-4?utm_source=openai)) This suggests that the quotes have been reused without significant modification, indicating a lack of originality.
Source reliability
Score:
4
Notes:
The narrative originates from the Daily Mail, a publication known for sensationalism and occasional inaccuracies. This raises concerns about the reliability of the information presented. The King’s College London report is a reputable source, but the Daily Mail’s involvement diminishes the overall reliability.
Plausability check
Score:
5
Notes:
The claims about KCL-HO-1i enhancing chemotherapy effectiveness are plausible and align with previous research from King’s College London. ([kcl.ac.uk](https://www.kcl.ac.uk/news/new-drug-combination-kick-starts-immune-system-to-fight-cancer-4?utm_source=openai)) However, the lack of new information and the recycling of older material suggest a lower plausibility score. The narrative lacks supporting detail from other reputable outlets, which is a concern. The tone and language used are consistent with typical scientific reporting, but the sensationalist headline raises questions about the narrative’s intent.
Overall assessment
Verdict (FAIL, OPEN, PASS): FAIL
Confidence (LOW, MEDIUM, HIGH): HIGH
Summary:
The narrative is a recycled version of a 2018 report from King’s College London, with minimal updates and identical quotes. The Daily Mail’s involvement raises concerns about the reliability of the information. The lack of new information and the recycling of older material suggest a lower freshness score. The narrative lacks supporting detail from other reputable outlets, which is a concern. The tone and language used are consistent with typical scientific reporting, but the sensationalist headline raises questions about the narrative’s intent.