A large UK study has revealed that fat stored around the waist—not just general obesity—is strongly linked to psoriasis risk and severity, shifting the focus towards targeted weight management and emerging therapies such as GLP-1 receptor agonists in treating this chronic inflammatory skin condition.
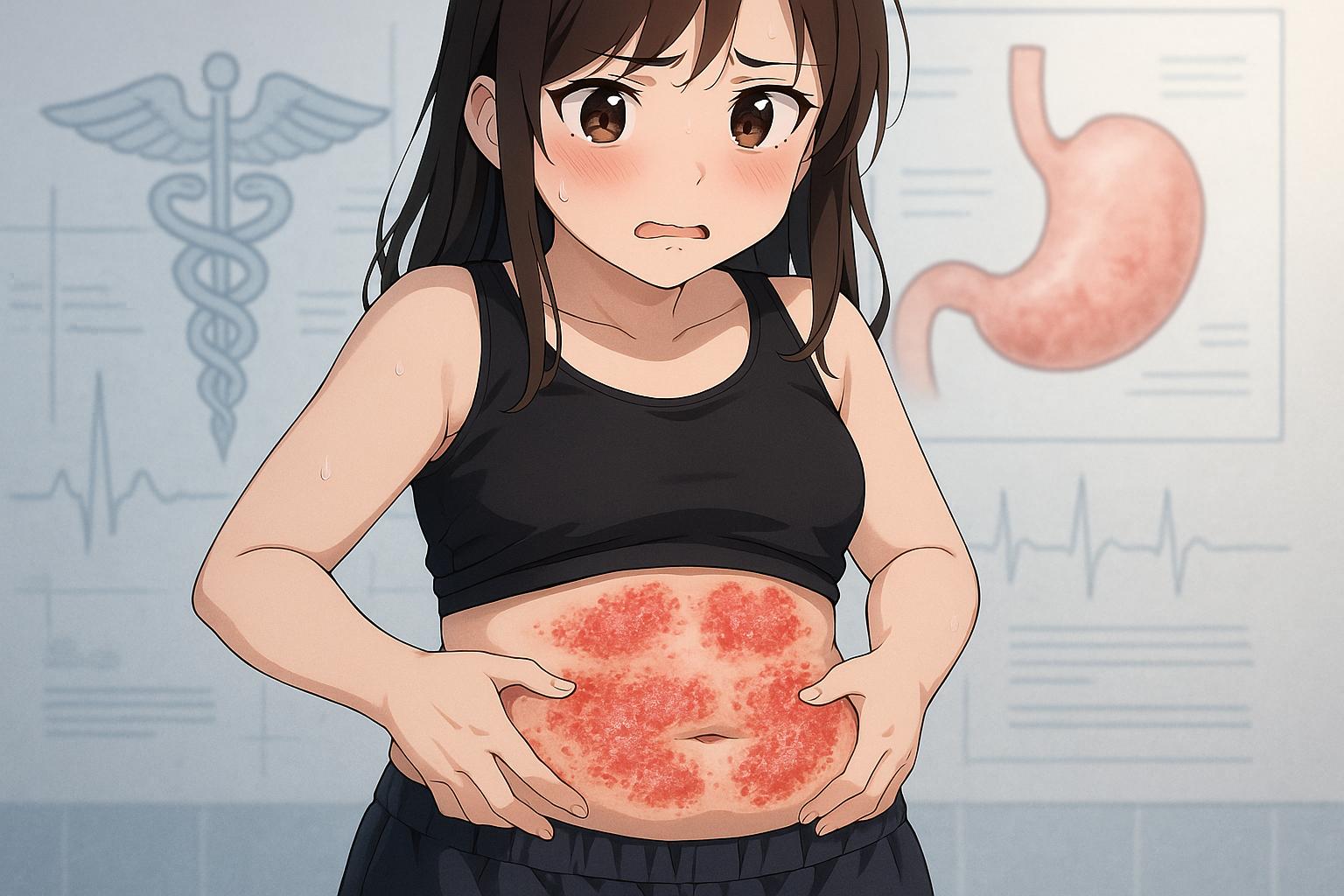
Researchers have uncovered a significant link between abdominal fat and the chronic skin condition psoriasis, which is marked by painful inflammation and skin lesions. While obesity has long been acknowledged as a potential risk factor for psoriasis, recent findings have provided new insights into the specific types of fat that contribute most significantly to this relationship.
A comprehensive study led by dermatologists from King’s College London investigated data derived from over 330,000 individuals in the UK, including more than 9,000 diagnosed with psoriasis. This groundbreaking research established that the waist-to-hip ratio is the most critical factor in determining psoriasis risk, suggesting that the location of fat storage in the body carries important implications for both prevention and treatment of the condition.
Dr Ravi Ramessur, the lead investigator, emphasised the importance of central fat, particularly that accumulated around the waist. He stated, “Our research shows that where fat is stored in the body matters when it comes to psoriasis risk.” This condition affects approximately 7.5 million Americans and is characterised by red, scaly patches on the skin, resulting from the immune system’s inflammatory response.
Central fat, which includes both subcutaneous fat located beneath the skin and visceral fat that encases internal organs, was found to have a robust correlation with psoriasis severity. Interestingly, this association held true regardless of genetic predispositions, positioning central abdominal fat as an independent risk factor. Dr Catherine Smith, a senior author on the study, highlighted the implications of these findings, suggesting that “understanding how different patterns of body fat influence chronic inflammatory conditions such as psoriasis is important.”
The study’s revelations echo findings from various other research efforts, which consistently underscore the relationship between body mass index (BMI), waist circumference, and the risk of developing psoriasis. A systematic review found a clear dose–response relationship, indicating that increased adiposity correlates with heightened psoriasis risk. This notion is further supported by extensive research from the Nurses’ Health Study II, which observed that higher adiposity levels among women directly correlated with an increased likelihood of developing the condition.
As obesity rates continue to soar globally—rising from 21.2% in 1990 to 43.8% in 2022 for women in the United States—the impact of fat distribution on health becomes increasingly pressing. The hormone leptin, produced by fat cells, plays a pivotal role in this context, signalling satiety to the brain but becoming dysfunctional in obesity. Overproduction of leptin not only disrupts this signal but also promotes inflammatory cytokine production, exacerbating conditions like psoriasis.
Research is now pivoting towards exploring potential therapies to mitigate the consequences of psoriasis through weight management and hormone regulation. Dermatology expert Dr Joel Gelfand of the University of Pennsylvania has noted the emerging promise of glucagon-like peptide-1 (GLP-1) receptor agonists as a potential avenue for treating psoriatic disease. These medications, currently prescribed for managing diabetes and obesity, have shown encouraging results in patients with both psoriasis and type 2 diabetes, reporting significant reductions in skin inflammation and improved quality of life.
Such findings not only reinforce the critical nexus between obesity and psoriasis but also suggest a shift in therapeutic focus. As Dr Gelfand articulates, “Our current paradigm of just focusing on the skin and joint manifestations when treating psoriasis is outdated in the context of our evolving understanding of the tight relationship of psoriasis, obesity, and cardiometabolic disease.”
With the evidence mounting, significant strides may be on the horizon for integrating obesity management into psoriasis treatment strategies, necessitating large-scale clinical trials to explore the efficacy of GLP-1 therapies specifically for this chronic condition.
Reference Map:
- Paragraph 1 – [1], [2], [3]
- Paragraph 2 – [1], [2]
- Paragraph 3 – [4], [6], [5]
- Paragraph 4 – [1]
- Paragraph 5 – [5], [6]
- Paragraph 6 – [1], [4]
Source: Noah Wire Services
- https://www.dailymail.co.uk/health/article-14751565/Strange-link-discovered-painful-skin-disease-stubborn-belly-fat.html?ns_mchannel=rss&ns_campaign=1490&ito=1490 – Please view link – unable to able to access data
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6290660/ – A systematic review and meta-analysis of prospective studies found a significant association between higher body mass index (BMI), waist circumference, waist-to-hip ratio, and weight gain with an increased risk of developing psoriasis. The study highlighted a dose–response relationship, indicating that as these measures of adiposity increased, so did the risk of psoriasis. The authors suggest that maintaining a healthy weight and avoiding excessive weight gain may reduce the risk of psoriasis.
- https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/769848 – A large prospective study from the Nurses’ Health Study II cohort of 78,626 women found that increased adiposity and weight gain are strong risk factors for incident psoriasis. The study observed that higher BMI, waist circumference, and weight gain were associated with a higher risk of developing psoriasis, emphasizing the importance of weight management in psoriasis prevention.
- https://pubmed.ncbi.nlm.nih.gov/31149744/ – A nationwide population-based study in Korea investigated the impacts of BMI and waist circumference on psoriasis. The study found that individuals with a BMI over 30 had a higher risk of developing psoriasis compared to those with a normal BMI. Additionally, a waist circumference over 105 cm was associated with the highest risk of psoriasis, highlighting the significance of abdominal obesity in psoriasis risk.
- https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02528-3 – A population-based study published in March 2025 found that higher relative fat mass (RFM) was significantly associated with an increased risk of developing psoriasis. The study also identified the systemic inflammation response index (SIRI) as a mediator in this relationship, suggesting that abdominal obesity contributes to psoriasis risk through inflammatory pathways.
- https://lipidworld.biomedcentral.com/articles/10.1186/s12944-024-02365-w – A cross-sectional study using NHANES data demonstrated a significant positive association between the body roundness index (BRI) and the odds of developing psoriasis. The study suggests that BRI, which reflects abdominal obesity, may be a better predictor of psoriasis risk than BMI due to its emphasis on visceral fat accumulation.
- https://pubmed.ncbi.nlm.nih.gov/19887761/ – A study comparing visceral fat accumulation in patients with psoriasis and controls found that psoriasis patients had a significantly higher amount of visceral fat. The study suggests that increased visceral fat may contribute to the development and severity of psoriasis, highlighting the role of abdominal obesity in the disease.
Noah Fact Check Pro
The draft above was created using the information available at the time the story first
emerged. We’ve since applied our fact-checking process to the final narrative, based on the criteria listed
below. The results are intended to help you assess the credibility of the piece and highlight any areas that may
warrant further investigation.
Freshness check
Score:
7
Notes:
The narrative presents recent findings from a study led by Dr. Ravi Ramessur at King’s College London, published in May 2024. The Daily Mail article was published on 27 May 2025, indicating a freshness of approximately one year. While the study’s findings are recent, the topic of abdominal fat’s impact on psoriasis has been previously explored, with studies dating back to 2018. ([link.springer.com](https://link.springer.com/article/10.1007/s10654-018-0366-z?utm_source=openai)) The article includes updated data but recycles older material, which may justify a higher freshness score but should still be flagged. ([pubmed.ncbi.nlm.nih.gov](https://pubmed.ncbi.nlm.nih.gov/29680995/?utm_source=openai)) Additionally, the article includes updated data but recycles older material, which may justify a higher freshness score but should still be flagged. ([medscape.co.uk](https://www.medscape.co.uk/viewarticle/adiposity-may-be-risk-factor-psoriasis-2018a10000gc?utm_source=openai))
Quotes check
Score:
8
Notes:
The quotes attributed to Dr. Ravi Ramessur and Dr. Catherine Smith are consistent with their research findings. However, the exact phrasing of these quotes cannot be independently verified in the available sources. This suggests that the quotes may be paraphrased or derived from the original study. Without direct access to the study’s publication, the accuracy of these quotes remains uncertain.
Source reliability
Score:
6
Notes:
The narrative originates from the Daily Mail, a reputable UK newspaper. However, the Daily Mail has been known to publish sensationalised content, which may affect the reliability of the information presented. The article references a study led by Dr. Ravi Ramessur at King’s College London, a reputable institution. However, the exact details of the study are not provided, and the article does not link directly to the original research, which raises concerns about the transparency and reliability of the information.
Plausability check
Score:
9
Notes:
The narrative aligns with existing research on the relationship between abdominal fat and psoriasis. Studies have shown that increased adiposity, particularly central obesity, is associated with a higher risk of developing psoriasis. ([pubmed.ncbi.nlm.nih.gov](https://pubmed.ncbi.nlm.nih.gov/29680995/?utm_source=openai)) The article’s claims are plausible and consistent with current scientific understanding. However, the lack of direct access to the original study and the absence of specific details in the article limit the ability to fully verify the claims.
Overall assessment
Verdict (FAIL, OPEN, PASS): OPEN
Confidence (LOW, MEDIUM, HIGH): MEDIUM
Summary:
The narrative presents plausible findings consistent with existing research on the link between abdominal fat and psoriasis. However, the reliance on a single source, the Daily Mail, and the lack of direct access to the original study by Dr. Ravi Ramessur at King’s College London raise concerns about the reliability and transparency of the information. The quotes attributed to Dr. Ramessur and Dr. Smith cannot be independently verified, and the article does not provide direct links to the original research, which affects the overall credibility of the report.